Racism Experienced During Pregnancy May Alter Infant Brain Circuitry. What Can We Do to Support BIPOC Moms and their Babies?

Abstract
Recognizing the connection between racism experienced during pregnancy, perinatal mental health and infant brain development is a first step in supporting the mental and physical wellbeing of BIPOC birthing parents and their children. Strategies that address inequity in health care settings, incorporate targeted prenatal interventions and strengthen collaboration among healthcare practitioners have the potential to improve outcomes.
Prenatal stressors — including discrimination — affect infant brain development
In late 2023, a group of Yale and Columbia University researchers published a study which showed that racism and racial discrimination experienced by women during pregnancy may affect their infant’s brain circuitry.
This study was based on self-reported instances of discrimination and acculturation in a sample of women where 88% of participants identified as Hispanic. We know that racial discrimination and acculturative stress can negatively impact a person’s physical and mental health. But this study went a step further, showing how changes in the brain were evident in MRI studies of the newborn babies of women who experienced discrimination.
In what way did the negative racial or cultural experiences of the mothers affect their infants’ brains? Adverse experiences are known to affect the amygdala, the portion of the brain associated with emotional processing. The amygdala is also believed to be involved in racial and ethnic processing. The researchers in this particular study found that prenatal discrimination had an effect unlike other prenatal stressors. The infants’ brains displayed weaker connectivity between the amygdala and the prefontal cortex, which is associated with higher-order functioning.
While the precise biological mechanisms involved in these changes are still being studied, the findings are not surprising given what we know about how prenatal stressors can affect the brain development of infants. Other research focused on “fetal programming” shows that prenatal stress can affect the fetal brain and future neurobehavioral development. For example, the placenta is responsible for regulating the chemicals and hormones that pass from the mother to the developing fetus. Maternal stress or trauma can actually change the way the placenta operates, in turn affecting the infant’s brain circuitry.
Prenatal stress disproportionately affects mothers and babies of color
All birthing parents regardless of background, may encounter prenatal stressors such as mental health challenges.
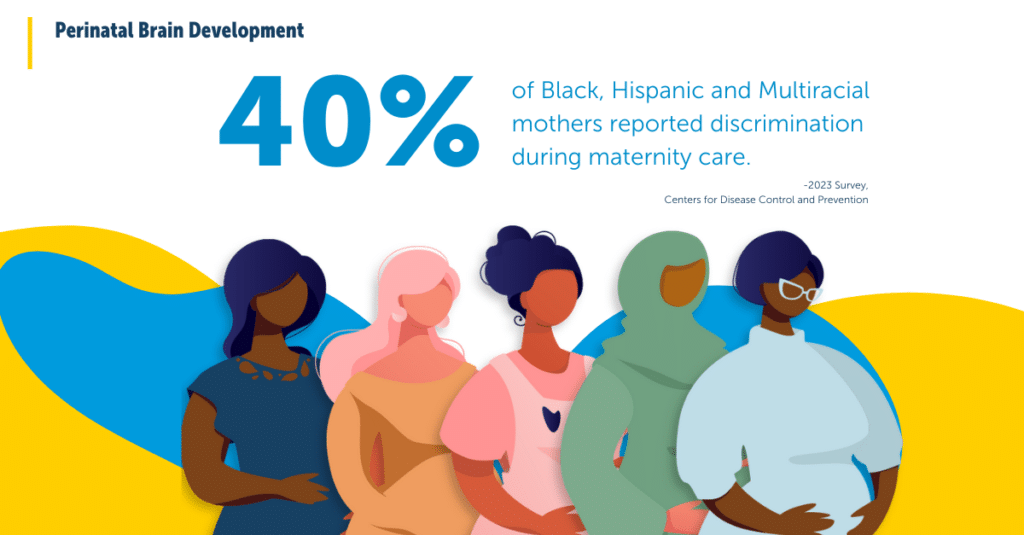
However, prenatal stress disproportionately affects women of color and their babies, and the racism that BIPOC women often experience is a major contributing factor. Experiences of everyday discrimination have been linked to maternal depression and mothers feeling unattached to their unborn children. In addition to everyday racism and structural racism in areas like employment or housing, another pervasive way that racism manifests during pregnancy is in discriminatory and inequitable treatment by healthcare professionals. This includes having health concerns ignored, treatments delayed or refused, or experiences of pain dismissed. In a 2023 survey analyzed by the CDC, approximately 40% of Black, Hispanic, and Multiracial mothers reported discrimination during maternity care.
Acculturative stress — the psychological challenge of adapting to a new culture and adopting new beliefs and customs — can lead to anxiety and depression for members of immigrant groups and was one of the prenatal stressors measured in the Harvard/Yale study. Black birthing parents may face another compounded stressor due to the unique experience of gendered racial stress. A 2022 study demonstrated that not only do Black women experience the stressor of racism during pregnancy, but they also experience a hybrid type of stress due to their intersecting social identities of race and gender.
How can we support BIPOC women experiencing prenatal stressors?
What can be done now to address the health needs women of color and their babies? In addition to working together to fix structural inequities, there are specific steps that we can take to support parents before birth:
- Supporting prenatal attachment. When parents-to-be undergo adverse experiences exacerbated by inequity and discrimination, they are more likely to experience depression and anxiety. This is linked to a lower quality of fetal attachment. There are several existing programs that work to support the relationship between parent and fetus, including the PREPP intervention which aims to treat women at risk for post-partum depression and promote infant health. This intervention builds on the work that the Perinatal Pathways Lab at Columbia University was doing in looking at the impact of pregnant women’s distress on fetal and infant brain–behavior development.
- Listening to pregnant BIPOC women and making them partners in decision-making about their own care and treatment plans. This includes recognizing and working to eliminate unconscious bias, as well as ensuring that all patients are respected and have their concerns taken seriously. For populations that have routinely been discriminated against in their maternal care and may be hesitant to speak up, it’s especially important to encourage patients to ask questions and share concerns.
- Building greater connections between mental healthcare practitioners, primary care, and maternal healthcare providers. Healthcare systems have historically separated care for mental and physical health, meaning that the doctors who see pregnant patients most frequently may not be the ones able to support them with mental health concerns. Some solutions to this disconnect have included perinatal psychiatry consultation lines for physicians, education for medical providers on screening for maternal depression, and the integration of perinatal mental health into home visitation and healthcare settings.


