How a New York Practice is Advancing Health Access in Pediatric Primary Care

Despite progress, health disparities still exist
In 2020, the US Department of Health and Human Services' has set an overarching goal of eliminating health disparities by 2030.
“We are almost halfway to 2030, and unlikely to see the elimination of health disparities, despite progress in some areas,” says Diane Lee, PsyD. The work must continue.
At the Division of General Academic Pediatrics at Weill Cornell Medicine, Diane Lee,
PsyD, Nancy Jade Lee, MD, and Rachel Wirtshafter sought to identify ways that they could advance health equity in pediatrics. Recognizing that as health professionals, they and their colleagues may be likely to recognize the broader disparities that exist in the world, but less attuned to the ways that disparities show up in their day-to-day activities, they decided to explore improvements in their setting and services that could move the needle.
Disparities are differences in the incidence, prevalence, mortality, burden, and experience of disease or health conditions that are observed among specific populations.
When it comes to health care disparities, research shows:
- Racial and ethnic minority patients experience lower strength of affiliation with providers and are more likely to experience interactions with health care providers as unhelpful and disempowering
- Patients from diverse language backgrounds experience higher rates of medical errors
- Almost 1/3 of African Americans reported personally experiencing racial discrimination during a visit with a health care provider and almost 1/4 avoided getting care due to fear of discrimination
- Children from racial and ethnic minority and language-diverse backgrounds are less likely to receive developmental and social-emotional screening
- Children from racial and ethnic minority and language-diverse backgrounds are less likely to receive a developmental delay diagnosis from their primary care physician
- Women from racial, ethnic, and language diverse backgrounds are the least likely to be screened for postpartum depression
Disparities begin very early on, even before birth. We see it in prenatal care, including rates of prematurity and low birthweight, infant mortality, and maternal mortality (three times higher for Black women). Overall, children of color have significantly higher rates of morbidity and mortality related to poor maternal, prenatal, and early childhood health.
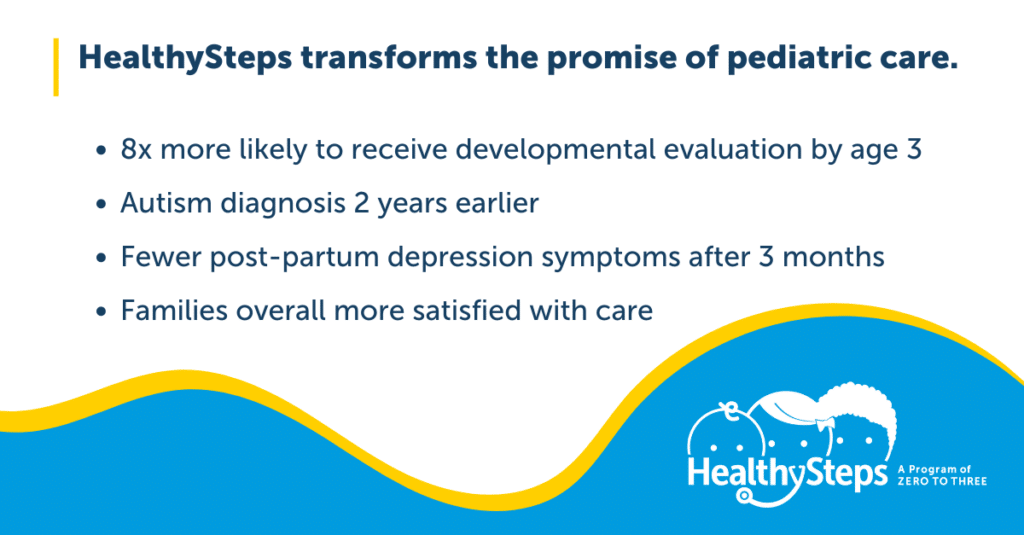
The team at Weill Cornell Medicine had heard about the proven success of HealthySteps in addressing health disparities in pediatrics and were eager to implement the model in their clinic.
An urban, academic residency teaching clinic affiliated with Weill Cornell Medicine, their practice has 40 pediatric residents and 8 attending physicians serving around 6,000 patients – with about 1,500 of these between the ages of 0 to 3. Within their patient base, 89% of our families identify as racial and ethnic minorities, 98% are publicly insured and 17% report a language other than English as their preferred language.
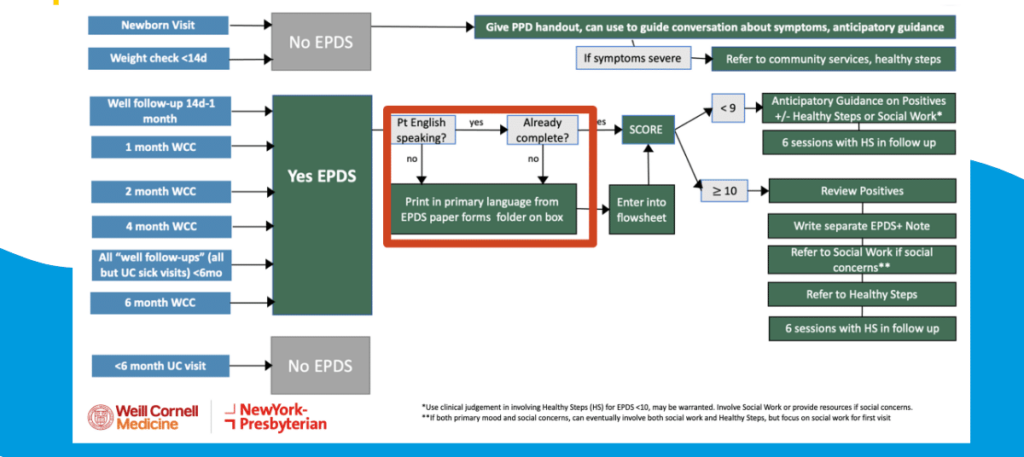
For maximum impact and better evaluation, the team decided to focus their efforts on one specific area: post partum depression screening. This screening is a key way that the providers identify whether families may benefit from HealthySteps, and are what often trigger the earliest point of referral.
Given our population, we wanted to make sure that our families that were unfortunately most likely to experience disparities in the health care system were the ones who were receiving the most or the highest level of HealthySteps services.
Diane Lee, PsyD
Improving access to quality care in pediatrics
Especially in the primary care setting, inadequate workflows and training can reinforce or worsen disparities in access to care
After some time implementing HealthySteps, the team reviewed their electronic health records data and saw that families receiving a higher level of support through HealthySteps were more likely to be English-speaking, compared to their overall patient population. This told them that they were likely missing families that could have benefited the most.
Untreated maternal depression and anxiety affect parent-child attachment and the healthy development of young children. African American and Hispanic mothers have the highest rates of postpartum depression among all racial and ethnic groups, but are less likely to receive treatment, due to lower screening rates and less successful referrals.
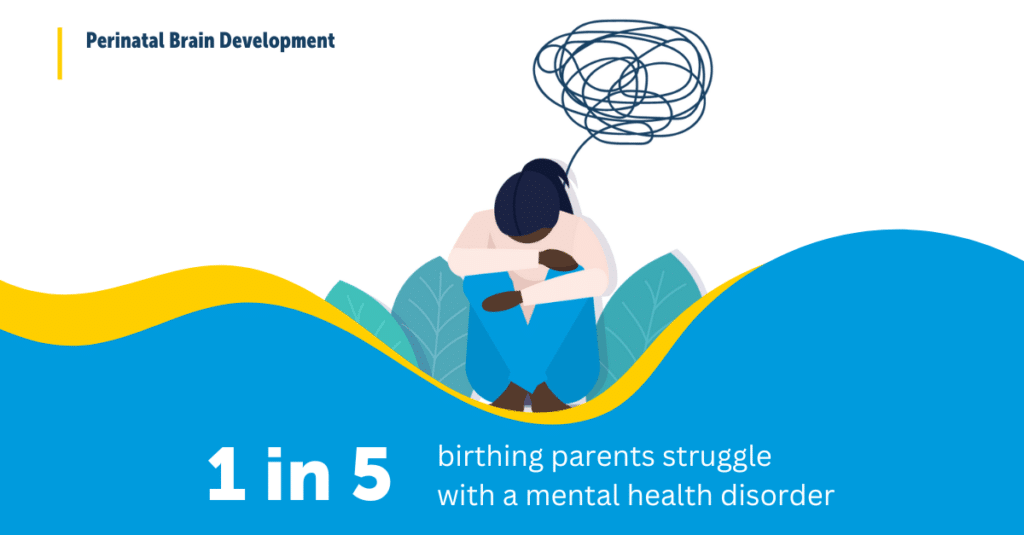
Learn more about the factors that contribute to poor maternal mental health, including discrimination and racism.
In the case of the Weill Cornell team, they identified several, interrelated factors that were likely contributing to the disparities in screening and referrals.
- Lack of clarity among key staff about what to do with a positive screening result
- The impact of a busy, often-chaotic work environment on a process with multiple touchpoints
- Language barriers among patients
- Patient comfortability in completing the screenings, due to lack of context
To address these factors, they developed and implemented new strategies to improve the practices’ workflow and ensure all team members – from front desk staff, to technicians, to nurses – were trained in best practices for administering the screenings. And because HealthySteps is a team-based program, the pediatricians and residents played a key role in training and supporting staff.
I used to think that process was simple but quickly learned that we really have to work together to make this happen and I could not do it by myself.
Diane Lee, PsyD
 While a part of the problem was not having screenings available in the necessary languages, the team realized that it was also about ensuring that the families understood why they were being asked these questions, and felt comfortable filling them out, as well as ensuring that the appropriate follow-up steps were taken if a screening returned positive, to ensure that the mom got the appropriate referral and care coordination.
While a part of the problem was not having screenings available in the necessary languages, the team realized that it was also about ensuring that the families understood why they were being asked these questions, and felt comfortable filling them out, as well as ensuring that the appropriate follow-up steps were taken if a screening returned positive, to ensure that the mom got the appropriate referral and care coordination.
“We had to take a step back and think about what it takes to get a screening from the iPad at the front desk into the family’s hands, then into the provider’s hands, then to the attending’s hands, and then to the HealthySteps Specialist,” says Diane.
Key Takeaway
This quality improvement initiative, including the implementation of HealthySteps, co-creating workflows, and changing note templates, increased the percentage of caregivers who were screened for postpartum depression. Additionally, this project decreased the gap in screening rates between English and non-English screens by increasing overall screening rates in caregivers whose preferred language is not English.
Proven improvements in access to quality pediatric healthcare
When we remove barriers and promote greater access to opportunity, flourishing is possible for everyone.
HealthySteps is a team-based approach, aimed at full practice transformation. At Weill Cornell’s pediatric resident clinic, the implementation of HealthySteps, including a dedicated HealthySteps Specialist, not only resulted in improved overall screening rates, but allowed for a deeper investigation and intervention toward reducing disparities in service delivery.
“My proudest moments are when our nurses or techs come in and ask any one of our residents about which screenings a patient should be getting and they don’t ask me, the HealthySteps Specialist. They know to ask any one of the providers because we are all responsible for screening together,” says Diane.
Thank you to the team at Weill Cornell for sharing their work so that others can learn from it.
Together, the national network of HealthySteps sites aims to reach more than 1 million young children and families annually by 2032.
Learn more about our work to prioritize family-centered, quality service delivery and reduce disparities.

Authors

Rachel is a public health professional currently working at Weill Cornell Medical Center as a Pedia…

Diane is a HealthySteps Specialist and has expertise in early trauma, parent management training, a…

Nancy is an assistant professor of clinical pediatrics at Weill Cornell Medicine and an assistant a…
Related Resources
References
Lee, D., Lee, N. J., & Wirshafter, R. (2024, August). HealthySteps, Uneven Ground: Addressing Service Disparities in Pediatric Primary Care. ZERO TO THREE’s 2024 LEARN Conference. Long Beach; CA.




