Alison D. Peak, Allied Behavioral Health Solutions, Nashville, Tennessee; Mindy Kronenberg, Memphis, Tennessee; Diana Morelen, East Tennessee State University; Carmen Rosa Noroña, Boston Medical Center, Boston, Massachusetts; Karen Frankel, University of Colorado-Denver; and Angela Webster, Association of Infant Mental Health in Tennessee
Abstract
The Tennessee First Five Training Institute (TFFTI) is a workforce development project to build infant and early childhood mental health (IECMH) capacity across Tennessee’s community mental health agencies. TFFTI focused on foundational trainings in IECMH concepts, training in child–parent psychotherapy, dyadic, trauma treatment for children birth to 6 years old, and reflective consultation. This article will discuss TFFTI’s programmatic shift in the wake of Tennessee’s March 3, 2021, tornado, COVID-19, and the murder of George Floyd. The authors highlight TFFTI’s collaborations with national partnerships to adapt training and provide support through virtual formats. The authors discuss lessons learned and provide guidance for others considering large-scale IECMH workforce development efforts.
At the beginning of 2019, Tennessee had less than 10 clinicians with more than 20 hours of training in clinical infant and early childhood mental health (IECMH). These individuals served 95 counties and more than 400,000 children under 6 years old (U.S. Census Bureau, 2021). The need for a cohesive workforce development plan was clear.
The Tennessee First Five Training Institute
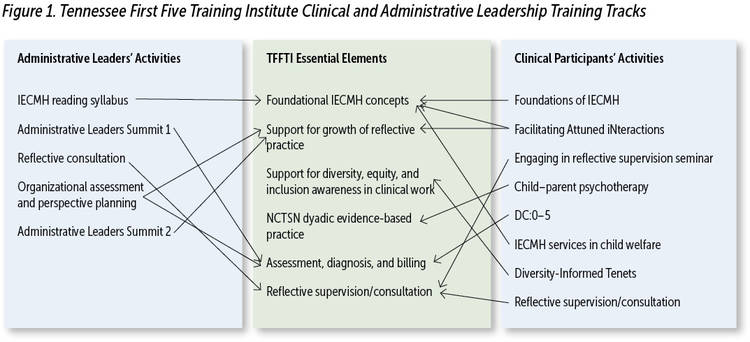
In 2019, Allied Behavioral Health Solutions (Nashville, Tennessee) received funds through the Department of Children’s Services Building Strong Brains Innovation grants to develop the Tennessee First Five Training Institute (TFFTI; Tennessee Department of Children’s Services, 2016). TFFTI differentiated itself through the provision of both clinical and administrative leadership training tracks (see Figure 1). The training protocol for the scope and depth of TFFTI identified six essential elements for participants of both tracks:
- training in foundational concepts such as Ghosts and Angels in the Nursery (Fraiberg et al., 1975; Lieberman et al., 2005);
- training to support reflective practice such as Facilitating Attuned Interactions (Heffron et al., 2016);
- training to emphasize the role of race and culture in work with young children and families through Diversity-Informed Tenets (Frankel et al., 2019);
- training in an evidence-based trauma treatment, child–parent psychotherapy (CPP; Lieberman et al., 2015);
- building awareness in the interconnectedness of systems to service delivery through assessment, diagnosis, and billing through the DC:0–5TM: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0–5; Mothander, 2016);and
- the necessity of consistent and frequent reflective consultation to support participants in integrating this depth of knowledge into their daily work.
Measures of Participant Change
Clinical participants completed the Curiosity and Exploration Inventory-II (Kashdan et al., 2009); Freiburg Mindfulness Inventory (Walach et al., 2006); an IECMH knowledge assessment scale; and the Provider Reflective Process Assessment Scale pre, mid, and 6 months post participation in the project (Heller, 2017; Kashdan et al., 2009; Michigan Association for Infant Mental Health, 2017; Walach et al., 2006). Administrative leadership completed an IECMH-adapted Organizational Readiness for Change Assessment (ORCA; Helfrich et al., 2009). Although outcomes of those measures are not the primary focus of this article, preliminary findings demonstrated that clinical participants showed statistically significant growth in IECMH knowledge assessment scale and that organizations demonstrated statistically significant change within the domain related to use of reflective supervision within organizations.
Participant Selection
In spring 2019, the Tennessee Association of Mental Health Organizations, the state’s advocacy organization for nonprofit community mental health centers, announced a bid for participants. Applying agencies selected three or four clinical providers to participate in the clinical cohort and two administrative leaders with decision-making power within the organization to participate in the Administrators’ cohort. Six agencies were selected to proportionally represent each of Tennessee’s three Grand Regions and to represent geographical proximity to Tennessee Safe Baby Courts. The selection of the six agencies resulted in a clearly identified clinical cohort (n = 19) and Administrators’ cohort (n = 12) across the six agencies.

An EF4 tornado had touched down in Nashville and another EF4 tornado touched down in nearby Cookeville. Photo: Phillip Fryman/shutterstock
Training Models and Goals
TFFTI intended to build IECMH knowledge and reflective capacity among both clinical and leadership participants and to track changes across both cohorts. The increased involvement of leadership was designed to help organizations to think critically about the adaptations that might be necessary to fully implement IECMH modalities. This model allowed for increased support of clinical providers and greater connection between providers and leadership (Noroña & Acker, 2016). Further, the cross-cohort education brought differing perspectives to the six essential elements of training. The metrics, data, and outcomes identified through the cohort are considerable, but outside the scope of this article and we hope to discuss them further in future publications.
Clinical Training Model
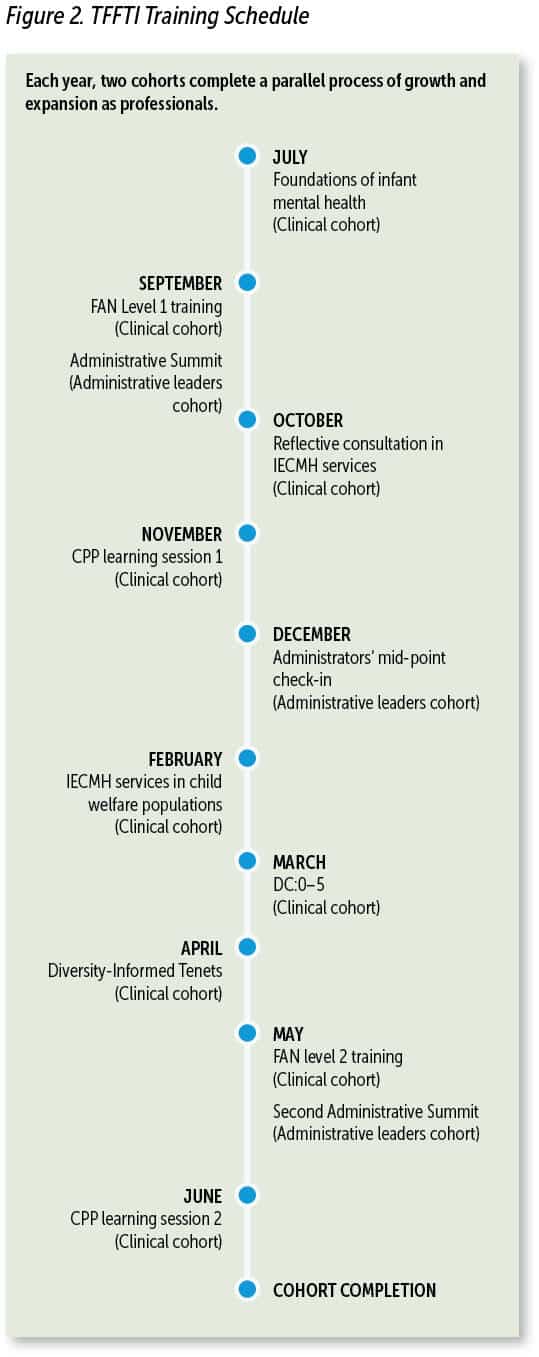
The clinical cohort was designed to engage participants in more than 40 hours of IECMH training and provide them with 48 opportunities for reflective consultation across the year-long cohort. TFFTI’s grounding clinical intervention is CPP (Lieberman et al., 2015). In addition to training in CPP, participants received training in Facilitating Attuned Interactions (FAN), DC:0–5 (ZERO TO THREE, 2016) and the Diversity-Informed Tenets for Work With Infants, Children, and Families (Irving Harris Foundation, n.d.).
The order and inclusion of these trainings (see Figure 2) allowed TFFTI to address the essential elements related to training in foundational concepts; training in reflective practices; training in an evidence-based trauma model; and training in systems work, assessment, and billing to support the CPP uptake and fidelity.
To address the essential element of reflective consultation and to meet the fidelity requirements for both FAN and CPP, TFFI engaged three regional consultants to provide weekly to biweekly reflective supervision and consultation to the participants from their respective Grand Regions. The groups ranged in size from 6 to 8 participants. This format allowed for participants to form a relationship with a local content expert as well as build relationships with other clinicians in their geographical area. These “regional groups” met weekly for the first 5 months of the training cohort and then moved to biweekly to allow for large group CPP consultation. The alternating format between smaller regional groups and the larger cohort allowed for consistent building of relationships, learning from different perspectives, and continuity among discussions.
Administrative Leadership Training Model
The Administrators’ cohort began by completing an IECMH-adapted ORCA (Kononowech et al., 2021), which was selected due to its self-report format and its consideration of multiple facets of organizational life. Respondents engage in a process of reflection on their organization across five domains: System’s Perception of IECMH Services, Organizational Capacity for Implementation, Functional Considerations, Organizational Culture/Climate, and Senior Leadership and Staff Development. Responses are plotted on an intersectional map that allows for the organization to clearly see their strength areas and growth edges (Helfrich et al., 2009). The maps were introduced at an Administrators’ Summit in the fall to prompt reflection on leadership and current organizational dynamics. The maps were then used as guides for technical assistance and reflection across the year-long cohort.
A second Administrators’ Summit was planned for late spring of 2020 to repeat the ORCAs and allow for reflection on organizational change and growth. The Administrators’ cohort also met biweekly for reflective consultation and received at least one technical assistance call between the two Administrators’ Summits. The structure of this cohort encouraged leadership to consider caseloads, billing practices, staff burnout, and their own experience of being leaders in large organizations.
The Space Between “No Longer and Not Yet”
On March 3, 2020, at approximately 4:30 am, one of the authors (ADP) was awoken by numerous calls and text messages inquiring about the safety and well-being of staff and clients’ families. In the hours and sunlight that followed it would become known that an EF4 tornado had touched down in Nashville and another EF4 tornado touched down in nearby Cookeville. The combination of the two tornadoes would take the lives of 25 individuals, injure 250, and prove to be the 6th costliest tornado series in U.S. history (Medina, 2021).
On March 5, 2020, the first case of COVID-19 was identified in Tennessee. By March 23, 2020, schools across all 95 counties were closed for, what ultimately would be, the remainder of the year (Tennessee Department of Health, 2020).

The virtual format of the training proved to be both a challenge and a blessing. Photo: Monkey Business Images/shutterstock
In the span of less than 48 hours, the predictable lives of those hosting and participating in TFFTI were dramatically changed. The ability to be together for upcoming trainings was thrown into uncertainty and the questions abounded. Reflective consultation groups had been provided in a virtual meeting format from the beginning to address geographical spread of participants. It quickly became apparent that reflective consultation was the constant that remained for both cohorts in the early weeks of COVID.
Clinicians were anxious about whether trainings would continue to be provided. Would they be able to complete the CPP rostering process they were working so diligently to achieve? What would their current services to families look like? Leaders asked about ways to support staff wellness. How would they keep staff safe? What cleaning protocols should be in place? In the beginning the answers generally consisted of “I don’t know.” “We’re working on it.” And “We’re in conversations with our national partners about what options there are.”
At that time, no virtual format existed for DC:0–5, FAN, Diversity-Informed Tenets, or CPP Learning Session 2, and these trainings still needed to be completed by the cohort prior to the end of the training year. The Administrators’ cohort faced additional pressure to provide guidance and answers to clinical staff and were looking to TFFTI as a resource in a time when no literature or model existed for leading an organization in the midst of natural disasters and national health crises at the same time. In an effort to continue hearing participants and promote reflective capacity as an essential element of the project, TFFTI leadership met to consider options to “be with” the participants in this time when it was no longer safe to be together in person. It was quickly apparent that connection and continuity would be imperative to addressing participant anxiety and supporting the continuation of services to young children and families.

As spring of 2020 continued, racial inequities were becoming more evident to the general public and more consistently discussed in mainstream media. Photo: Jelani Photography/shutterstock
Throughout TFFTI’s shift from in-person training to a virtual format, two key quotes were anchoring guides in the midst of such uncharted waters. A quote from a colleague at FAN National Network meeting referenced that COVID-19, and for Tennesseans the associated natural disasters, had called professionals and families alike into “the space between no longer and not yet” (K. Connors, personal communication, April 2020). Within a few weeks of this quote, Dr. Alicia Lieberman provided her Haruv lecture and discussed how the ocean in its many forms provides both intrigue, excitement, and fear for everyone at different depths (2020). This idea that TFFTI was forging through these waters with other colleagues across the world in efforts to support those clinicians and the clients they served locally was a driving (and comforting) force in the days between March and June of 2020.
Collaboration With National Faculty to Adapt Training
The collaborative efforts of colleagues and experts across the US ensured that TFFTI’s participants received the training they were promised and that there would be continuity to anchor participants in the midst of such uncertainty (see Table 1).
The program developers and trainers for FAN, DC:0–5, Diversity-Informed Tenets, and CPP held numerous conversations about adapting the training. None of these models had, to date, hosted their trainings in a virtual format. There was deep concern that the material may not translate as well on a virtual platform as it did in person. Activities and learning points would have to be shifted and re-worked to accommodate breakout rooms and whiteboard features. There were questions as to whether trainings could continue to host as many seats as had been considered for in-person options. And at the center of all these anxieties lay the real concern that the intentionally relational nature of this work would be lost, that the possibility of “being with” by videoconference might not be possible at all.
The supportive nature of the consistent reflective consultation that TFFTI’s leadership received throughout this process was integral to continuing conversations, allowing space for problem solving, and to consider how these questions might be addressed. This experience provided further evidence for the role of the parallel process in IECMH work. Participants remarked that this new virtual way of being together was supportive to them and helped them to understand that their new way of being with families would be supportive as well.
FAN Training Adaptations
In late May 2020, in collaboration with Dr. Linda Gilkerson and the Erikson Institute, the first iteration of FAN Level II training was hosted. The training was divided into 3-hour sections across 2 days instead of the original 1-day format. TFFTI participants joined by videochat and were greeted with the anchoring themes of FAN’s ARC of Engagement and Mindful Self-Regulation (Heffron et al., 2016). This training occurred just weeks after the murder of George Floyd and was the group’s first time to be together at large to consider the implications of police brutality and the clear disproportionate impact of COVID-19 on communities of color and communities below the poverty line. The FAN training was focused for these 2 days on intentional consideration of these then-current events and their role in our work as IECMH clinicians.
TFFTI participants were prompted to reflect on their own experience of race, how their identified race was a factor in the services they provided, and how to use the FAN as a tool during conversations of race and equity. The virtual format of the training proved to be both a challenge and a blessing. Participants were able to be together and to engage in extended conversation for the first time since quarantine had been implemented. The ability to connect, in whatever format was possible, felt like water to a thirsty soul. Through this initial experience, TFFTI and its national supporters began to see that maybe relationship was possible virtually, after all.
DC:0–5 Training Adaptations
In early June 2020, TFFTI partnered with ZERO TO THREE to pilot the first virtual iteration of the DC:0–5 training. Three Tennessee state-trainers collaborated with Kathleen Mulrooney, the program director of IEMCH from ZERO TO THREE, to consider the adaptions and implementations that would be required for the DC:0–5 training to remain both weighted with information and digestible in the electronic format. ZERO TO THREE’s DC:0–5 dissemination team worked to consider the electronic and learning needs of both participants and trainers. The state-trainers collaborated to create technical agendas ensuring that ZERO TO THREE’s efforts were detailed in a manner that allowed for smooth delivery of the training materials.
The initial iteration of the virtual training was conducted in two half-days with a 3rd 2-hour meeting approximately a week after the half-day trainings. The training was adapted from the DC:0–5 extended day format, which allowed for information to be covered in a sequential manner that reduced overall time in front of the screen and increased the didactic portion of the training into the first two training contacts. Participants were given a vignette between the 2nd and 3rd meetings to consider and attempt a diagnostic conceptualization. For the 3rd meeting, participants returned with their attempted diagnostic conceptualizations and then worked in breakout rooms with trainer support to consider their varying perspectives and arrive at an agreed-upon presentation. This format allowed for participants to be actively involved in the training material and to consider ways in which it would be applicable in their own work and agencies. The ability for participants to engage in a group diagnostic experience to complete the five axes found in DC:0–5 sparked many of those clinicians to later lead efforts within their agencies to adapt Electronic Health Records and to support state efforts for accepting the DC:0–5 as the appropriate nosology for treatment of children birth through 5 years old.
Diversity-Informed Tenets Training Adaptations
In mid-June of 2020, TFFTI partnered with the Irving Harris Institute and Diversity-Informed Tenets trainers to consider the provision of a Diversity-Informed Tenets training in a virtual format. Likely more than any other training that was adapted in conjunction with TFFTI, Diversity-Informed Tenets held an especially tenuous position in moving virtually. As spring of 2020 continued, racial inequities were becoming more evident to the general public and more consistently discussed in mainstream media. The need to provide this training was imperative and yet the Tenets training has always been a deeply reflective, relational experience. The Tenets have long sought to create open space for dialogue in which participants are encouraged to engage in self-reflection on their own awareness of race and equity as defined in Tenet 1 and also to explore Tenets 2 through 10 (see Box 1).
Box 1. The Diversity-Informed Tenets for Infants, Children and Families
- 1. Self-Awareness Leads to Better Services for Families
- 2. Champion Children’s Rights Globally
- 3. Work to Acknowledge Privilege and Combat Discrimination
- 4. Recognize and Respect Non-Dominant Bodies of Knowledge
- 5. Honor Diverse Family Structures
- 6. Understand That Language Can Hurt or Heal
- 7. Support Families in Their Preferred Language
- 8. Allocate Resources to Systems Change
- 9. Make Space and Open Pathways
- 10. Advance Policy That Supports All Families
Source: Irving Harris Foundation. (n.d.).
Meetings were held between Tenets staff, facilitators, and TFFTI leadership to consider the experiences and content that felt most salient both to the experience and in the cultural climate of those months. Considerations for inviting and supporting difficult conversation were given special attention. Further, there was early consideration for the idea of “videoconference fatigue” and how to keep participants engaged in the conversation in the midst of being, at that point, almost 3 months into a totally remote world. Ultimately, it was decided to limit the number of participants to 20 in order to promote connection and conversation. The Diversity-Informed Tenets facilitators focused intentionally on Tenet 1, Self-Awareness Leads to Better Services for Families, to provide participants with a singular grounding focus and to introduce the Tenets in a manner to encourage interest and further personal investigation of the Tenets (Frankel et al., 2019). Trainers also shared readings, resources, and personal reflective activities which were printed and mailed to participants to allow them the opportunity to engage actively in the Tenets experience and feel a sense of connection with what would have been anchoring aspects of an in-person training.
CPP Training Adaptations
In late June 2020, TFFTI held the 2nd CPP learning session in a virtual format. Implementation-level CPP training, which is based on National Child Traumatic Stress Network’s (NCTSN) learning collaborative model, is an 18-month process that, prior to the pandemic, included three in-person trainings: an initial 3-day learning session followed by two 2-day booster sessions at 6-month intervals. The booster sessions offer clinicians, supervisors, and administrators an opportunity to reflect on participants’ CPP cases through guided discussions, to gain a deeper understanding of CPP concepts, and to consider CPP implementation by learning from the successes and challenges of others.

Trainers were concerned that the relationship-based learning required for a relationship-based treatment model would not easily translate to a virtual format. Photo: Creative Minds2/shutterstock
Since March 2020, CPP national trainers and the CPP Dissemination Team from the Child Trauma Research Program at the University of California, San Francisco considered how to translate in-person CPP learning sessions to videoconference. Similar to issues that emerged with other IMH trainings, CPP trainers were concerned that the relationship-based learning required for a relationship-based treatment model would not easily translate to a virtual format. In addition, trainers were aware that a trauma-informed approach was required in translating a trauma treatment training to virtual. Issues to consider included the confidential nature of the case material and the recognition that many participants would be attending the training with their children at home. Further, CPP training leads participants to be rostered on a searchable database for families, courts, and other referral sources to use when selecting treatment providers. It was therefore important that the quality of the training not be diminished, and trainers were aware that participants may face multiple demands while learning from home. With these challenges in mind, the Dissemination Team moved forward in supporting CPP trainers to offer trainings virtually, noting the parallel process of training by videoconference as clinicians were learning to provide treatment by telehealth.
The timing of the TFFTI training offered unique challenges as many trainings were pushed back, and it was not feasible for participants to take off 4 half days of work to attend the training. Rather than hold the training later, the trainers split the training into 2 half-days several months apart. While this is not common practice, it was important to be flexible and not delay the learning process. The training included a 30-minute check-in each morning to simulate the space that emerges when participants arrive for an in-person training. Trainers opened the first day by acknowledging the current context and associated challenges for clinicians’ reflective practice and for the families they serve. The CPP core concept of integrating a sociocultural lens was highlighted by including Diversity-Informed Tenets and focusing on recognizing and intervening in diversity-related ports of entry, and both trainees and trainers shared recent examples in which conversations related to racism and police brutality emerged during CPP sessions. At the end of the training, the majority of participants reported satisfaction with the virtual format, with several reporting surprise having not expected to enjoy a training by videoconference.
Support for Organizational Administrators Through Administrators’ Summit
In mid-April, TFFTI shifted the intended Administrators’ Summit day to a series of 1.5-hour meetings across 4 consecutive weeks. TFFTI leadership engaged an out-of-state consultant to assist in the development of the collaborative series focused on topics such as identifying staff emotional responses to quarantine, transitioning IECMH services to telehealth platforms, and communal care for leaders. In surveys leading up to the 4-week series, 83% of the administrators reported that they strongly agreed that staff and colleagues needed more from them both professionally and emotionally and more than 65% of administrators felt that their positions required additional flexibility and new job expectations. However, in surveys following the 4-week series 100% of administrators reported that the series created a space where they felt concerns were heard and respected. The 4-week series was highlighted by a segment in collaboration with the Tennessee Department of Health’s medical director for Vaccine-Preventable Diseases and Immunization Program. This opportunity allowed for leaders to discuss concerns about cleanliness needs, protocols to ensure the well-being of staff and clients, and to consider the adaptations that were being requested of both administrators and staff. Administrators also echoed that this opportunity allowed for them to feel connected to those in positions to make decisions for the state as COVID-19 unfurled. Participants described their sense of connectedness in terms of feeling heard and being able to slow down in the process of making decisions for their own agencies. They expressed increased trust in the recommendations shared from Tennessee Department of Health.
Conclusion
In launching the TFFTI, the leadership team and TFFTI’s supportive partners (Association of Infant Mental Health in Tennessee, BlueCare of Tennessee, and the Tennessee Association of Mental Organizations, specifically) knew that there was much to be learned. However, the knowledge and experiences that resulted from the middle Tennessee tornados and COVID-19 surpassed our expectations of challenges, and subsequently, the depth of the lessons learned. By continuing to ground in the wisdom, relationships, and reflection within the IECMH community, TFFTI was able to successfully collaborate with several national partners to adapt in-person trainings to successful virtual experiences that allowed for continued support and growth of the participating mental health clinicians and administrative leaders. The weekly consultation calls and predictable schedule of training events allowed for continued connection for participants and a space to share together their personal and professional experiences during this time. This group was joined together in a manner that was unanticipated in the original design of TFFTI. This connection occurred likely in part due to the shared survival of the tornadoes, COVID-19, and marked awareness of racial inequity and injustice and of the shared calling to hold space for children and families as they too navigated this new realm.
The initial TFFTI cohort owes great thanks to leadership and trainers from Association of Infant Mental Health in Tennessee, FAN, DC:0–5, Irving Harris Diversity-Informed Tenets, and CPP for their willingness to “be with” TFFTI and to engage actively in relationship during a time of such stress and change. TFFTI’s second cohort was launched in July 2020 with the intention of being exclusively virtual. Without the experiences and collaboration that occurred in Cohort 1, Tennessee’s efforts to build clinical IECMH workforce capacity would have been at a stalemate. Ultimately, being present, being actively engaged in relationship, and being willing to walk uncharted waters together were the essential pieces to moving forward Tennessee’s efforts to improve IECMH access for its children and families.
Acknowledgment
TFFTI would like to acknowledge Lisa Asbill, Giovanni Billings, Chandra Ghosh Ippen, Kerith Hopper, Amanda Hwu, Stacey Leakey, Kathleen Mulrooney, Deb Peak, Sherryl Scott-Heller, and Nicole Tefera, who each played essential roles in TFFTI’s ability to adapt in the wake of COVID-19. TFFTI also acknowledges the contributions of one of the administrative leaders, Andrea Chase, who lost her battle with COVID in 2020. Her thoughts and perspectives were invaluable to Tennessee’s IECMH workforce development.
Authors
Alison D. Peak, MSW, LCSW, IMH-E®, is the executive director with Allied Behavioral Health Solutions and a licensed clinical social worker. Ms. Peak has spent the majority of her career dedicated to two primary passions: integrated behavioral health services in primary care settings and infant mental health. She has a master’s degree in social work from the University of Michigan and two post-graduate certificates: integrated behavioral health in primary care settings and pediatric integrated behavioral health. Clinically, Ms. Peak works primarily with children birth through 5 years old within the child welfare system. She collaborates across Tennessee and nationally to build programs that are responsive to gaps within the infant and early childhood mental health service delivery system. Ms. Peak was a founding board member of the Association of Infant Mental Health in Tennessee and is privileged to be a member of the 2020–2022 class of ZERO TO THREE Fellows.
Mindy Kronenberg, PhD, IMH-E®, a clinical psychologist in private practice in Memphis, Tennessee, specializes in infant mental health and the assessment and treatment of trauma across the lifespan. She completed the Irving Harris Infant Mental Health Fellowship at Louisiana State University Health Sciences Center, where she previously served as assistant professor. Dr. Kronenberg has provided crisis intervention as well as direct and consultative services in multiple settings including state agencies, schools, Head Start, dependency courts, and child welfare agencies. Dr. Kronenberg provides national training on evidence-based and evidence-informed assessments, practices, and treatments including child–parent psychotherapy, psychological first aid, reflective supervision, and relationship-based assessment. Dr. Kronenberg is a National Child Traumatic Stress Network (NCTSN) affiliate member and a past co-chair of NCTSN’s Zero to Six Workgroup. She was a founding board member of the Association of Infant Mental Health in Tennessee and is currently the group’s endorsement co-chair and member of the Advisory Council.
Diana Morelen, PhD, IMH-E®, is an assistant professor in the Department of Psychology at East Tennessee State University (ETSU) and a licensed clinical psychologist with specialization in infant mental health and perinatal mental health. Dr. Morelen is a clinical scientist committed to breaking the intergenerational transmission of trauma, adversity, and mental illness through evidence-based prevention and intervention programs. Dr. Morelen serves as a member of ETSU’s Strong BRAIN Institute, a board member for the Tennessee chapter of Postpartum Support International, and a regional lead for the Association of Infant Mental Health in Tennessee. Dr. Morelen’s work uses a trauma-informed, relationship-based, and diversity-informed approach to promote resilience from the top down (e.g., systems-level change) as well as the bottom up (e.g., community-based intervention programming).
Carmen Rosa Noroña, LICSW, MSW, MEd., IECMH-E®, is the child trauma clinical services and training lead at Child Witness to Violence Project at Boston Medical Center. She is a child–parent psychotherapy national trainer, an expert faculty of the DC:0–5TM: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0–5), and one of the developers of the Harris Professional Development Network Diversity-Informed Tenets for Work With Infants, Children, and Families Initiative ( https://diversityinformedtenets.org) and of the Boston Medical Center Family Preparedness Plan for Immigrant Families. Her practice and research interests are on the impact of trauma on attachment; the intersection of culture, immigration and trauma; diversity-informed reflective supervision and consultation; and on the implementation and sustainability of evidence-based practice in real-world settings. Ms. Noroña is a co-leader of the Department of Pediatrics Council of Social Justice, Diversity, Equity and Inclusion at Boston Medical Center. In addition, she serves as core faculty of the National Child Traumatic Stress Network’s (NCTSN) Being Anti-Racist Is Central to Trauma-Informed Care Initiative and as a member of the NCTSN Steering Committee. Ms. Noroña has adapted and translated materials for Spanish-speaking families affected by trauma and has also contributed to the literature in infant and early childhood mental health, diversity, and immigration.
Karen Frankel, PhD, is associate professor of psychiatry at the University of Colorado School of Medicine and director of the Harris Program in Child Development and Infant Mental Health. Dr. Frankel is a licensed clinical psychologist who has specialized in the assessment and treatment of young children for more than 30 years. She is the supervising psychologist for the University of Colorado Young Child Clinic, the executive director for Fussy Baby Network Colorado, and a national trainer for the DC:0–5TM: Diagnostic Classification of Mental Health and Developmental Disorders in Infancy and Early Childhood. Dr. Frankel received her bachelor’s degree from Oberlin College and her doctoral degree in clinical psychology from Indiana University. She completed an internship at the University of Washington School of Medicine and a postdoctoral fellowship through the Developmental Psychobiology Research Group at the University of Colorado School of Medicine
Angela Webster, MSW, IMH-E®, is executive director for the Association of Infant Mental Health in Tennessee (AIMHiTN). Ms. Webster spent the initial years of her career working in early childhood education and has a strong background in policy and grassroots advocacy, beginning with her work providing administrative oversight for an international child and community development organization. During her time with the agency, she oversaw organizations across several states whose focuses were families with children birth to 18 years old living in extreme poverty. Immediately prior to her transition to AIMHiTN, Ms. Webster was director of public policy for Disability Rights Tennessee, where she spent nearly 7 years leading the public policy team and building the agency’s capacity to impact systems change at all levels. She received her bachelor of social work degree from Northeastern State University in Oklahoma and her master’s of social work from Austin Peay State University through the Middle Tennessee Collaborative MSW Program.
Suggested Citation
Peak, A. D., Kronenberg, M., Morelen, D., Noroña, C. R., Frankel, K., & Webster, A. (2021). Being with…by Zoom?: Tennessee’s story of continuing IECMH workforce support and development in the time of COVID-19. ZERO TO THREE Journal, 41(4), 58–66.
References
Fraiberg, S., Adelson, E., & Shapiro, V. (1975). Ghosts in the nursery: A psycho- analytic approach to the problems of impaired infant-mother relationships. Journal of American Academy of Child Psychiatry, 14(3), 387-421.
Frankel, K., Njoroge, W., & Norona, C. R. (2019). The diversity-informed tenets for work with infants, children, and families: A tool for promoting diversity-informed clinical practice. Journal of the American Academy of Child and Adolescent Psychiatry, 58(10), S383.
Heffron, M. C., Gilkerson, L., Cosgrove, K., Scott Heller, S., Imberger, J., Leviton, A., Mueller, M., Norris-Shortle, C., Phillips, C., Spielman, E., & Wasserman, K. (2016). Using the FAN approach to deepen trauma-informed care for infants, toddlers, and families. ZERO TO THREE Journal, 36(6), 27–35.
Helfrich, C., Yu-Fang, L., Sharp, N., & Sales, A. (2009). Organizational Readiness for Change Assessment (ORCA): Development of an instrument based on the Promoting Action on Research in Health Services (PARIHS) Framework. Implementation Science, 38.
Heller, S. (2017). The Provider Reflective Practice Assessment Scale [Unpublished instrument]. Tulane University.
Irving Harris Foundation. (n.d.). Diversity-informed tenets for work with infants, children, and families. link
Kashdan, T. B., Gallagher, M. W., Silvia, P. J., Winterstein, B. P., Breen, W. E., Terhar, D., & Steger, M. F. (2009). The Curiosity and Exploration Inventory-II: Development, factor structure, and initial psychometrics. Journal of Research in Personality, 43, 987–998.
Kononowech, J., Hagedorn, H., Hall, C., Helfrich, C., Lambert-Kerzner, A., Miller, S. C., Sales, A., & Damschroder, L. (2021). Mapping the Organizational Readiness for Change Assessment to the consolidated framework for implementation research. Implementation Science Communications, 2(19).
Lieberman, A. F. (2020) Parenting under stress: What young children need to thrive in dangerous and uncertain times [Video]. Haruv from the Couch. link
Lieberman, A. F., Padrón, E., Van Horn, P., & Harris, W. W. (2005). Angels in the nursery: The intergenerational transmission of benevolent parental influences. Infant Mental Health Journal, 26(6), 504–520. link. PMID: 28682485
Lieberman, A. F., Ghosh Ippen C., & Van Horn. P. (2015). Don’t hit my mommy!: A manual for child–parent psychotherapy with young children exposed to violence and other trauma. ZERO TO THREE.
Medina, D. (2021, Jan 9). Tennessee tornadoes join record-breaking list of billion dollar natural disasters in 2020. The Tennessean. link
Michigan Association for Infant Mental Health. (2017). Competency guidelines for endorsement for culturally sensitive, relationship-focused practice promoting infant and early childhood mental health.
Mothander, P. (2016). DC:0–5TM: Diagnostic classification of mental health and developmental disorders of infancy and early childhood (DC:0–5) implementation considerations and clinical remarks. Infant Mental Health Journal, 37(5), 523–524.
Noroña, C. R., & Acker, M. (2016). Implementation and sustainability of child-parent psychotherapy: The role of reflective consultation in the learning collaborative model. Infant Mental Health Journal, 37(6), 701–716.
Tennessee Department of Children’s Services. (2016). Building Strong Brains TN ACEs. link
Tennessee Department of Health. (2020). TDH announces first case of COVID-19 in Tennessee. link
U.S. Census Bureau. (2021). Tennessee quickfacts. link
Walach, H., Buchheld, N., Buttenmuller, V., Kleihknecht, N., & Schmidt, S. (2006). Measuring mindfulness—The Freiburg Mindfulness Inventory (FMI). Personality and Individual Differences, 40(8), 1543–1555.
ZERO TO THREE. (2016). DC:0–5TM: Diagnostic classification of mental health and developmental disorders of infancy and early childhood.