Jennifer M. Moran and Mary Margaret Gleason, Eastern Virginia Medical School and Children’s Hospital of The King’s Daughters, Norfolk, Virginia
Abstract
The expanded scope of Axis III in DC:0–5 Diagnostic Classification offers opportunities to consider the influence of children’s physical health status on their mental health clinical presentation. Physical health conditions may influence children’s mental health through direct physiologic processes or indirectly by affecting a child’s experiences or the caregiver’s perceptions of the child. Health conditions may also provide information about the child’s caregiving environment. Many infant and early childhood mental health clinicians have limited training in a systematic approach to the review of a child’s physical health history and of the review of a health record. Electronic health records contain immense volumes of information about young children’s health. As a complement to history from caregivers, strategic review of the health record can yield valuable information that can inform the diagnosis and clinical formulation. This article provides a systematic approach to extracting relevant physical health information from an electronic health record and mapping these elements into the DC:0–5 diagnostic approach.
All children seeking mental health evaluation present with emotions, bodies, and relationships, all of which occur within the context of a child’s caregiving and cultural context, life experiences, and developmental status. A strength of the DC:0–5TM: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0–5; ZERO TO THREE, 2016) is the inclusion of a multiaxial system (see Jargon Buster, page 99), which includes explicit attention to health conditions and other physical health factors (Axis III) that may influence a child’s clinical mental health status. The importance of Axis III conditions are particularly relevant in early childhood mental health. First, emotional and behavioral changes and symptoms may reflect an infant or young child’s physical discomfort or distress, and attention to this possibility allows for the development of a treatment plan to address the underlying cause(s). In addition, infants and young children with mental health conditions experience physical health conditions at higher rates than others (Gleason et al. 2011). Older children with mental health concerns have higher rates of unmet physical health needs compared to other children, highlighting the importance of mental health professionals’ being attuned to ensuring that physical health concerns are recognized and treated (Bell et al., 2010).
In the field of infant and early childhood mental health (IECMH), the majority of clinicians have limited training in the physical health factors that influence mental health. Consideration of Axis III diagnoses does not require that an IECMH clinician becomes a physical health clinician or expand the scope of their practice. However, use of Axis III does require an IECMH clinician to consider the whole child, take a history that includes physical health factors, and collaborate with physical health providers to confirm the impact of the Axis III diagnoses on IECMH as needed.
DC:0–5 Axis III Framework
DC:0–5 highlights a number of mechanisms by which young children’s physical health conditions can influence mental health and the clinical issues that bring young children to seek mental health evaluations (ZERO TO THREE, 2016). First is the direct impact (see Table 1). Physical health conditions can directly influence mental health through the central nervous system (e.g., seizures); impact of physiologic effects of medications or toxins; and by causing discomfort, like pain or itching, which then can shape emotional regulation, behavior, or both. Physical health conditions can indirectly influence mental health clinical symptoms through the child or the caregivers’ experiences of the condition. For example, a child with immunocompromise may develop mental health symptoms through the limitations of their activities and interactions, or because the caregiver may protect the child so much that they do not support developmentally normative exploration. A physical health condition that confers immunocompromise may shape the caregiver’s perception of the child’s vulnerability or caregivers’ sense of responsibility for the child’s suffering, which may also influence the child–caregiver’s relational context (Axis II). Lastly, sometimes a physical health condition like a non-accidental injury may be a representation of an adverse caregiving environment. Notably, the absence of physical health concerns may also have important implications for IECMH in that physical health is associated with resilience.
Table 1. Mechanisms of Physical Health Influence on Infant and Early Childhood Mental Health Concerns
Diagnoses listed in Axis III can be specified as “acute” “chronic,” or “history of” in recognition of the potential for longstanding effects of a resolved physical health condition. IECMH clinicians should apply the Axis III diagnoses within the scope of their training. All clinicians should include the history of physical health concerns provided by the parent, along with diagnoses in available medical records. If a technical term for the condition is not available, the caregiver’s own words can be documented in quotations. A clinician may want to use phrases like “rule out” if substantial questions exist about the validity of a diagnosis. An IECMH clinician who observes possible signs of an Axis III condition as part of the assessment may describe their observations, such as “not using left arm,” and those with a physical health scope of practice may use a more specific diagnosis (e.g., “rule out cerebral palsy”).
Using the Electronic Health Record
When available, an electronic health record (EHR) can offer valuable information that may be efficiently extracted in preparation for an IECMH evaluation and diagnostic assessment. While the specific nomenclature of each EHR varies, the elements described here are available in most EHRs. EHRs offer some advantages in extracting valuable information about a child and family’s history. Health histories can be sorted, often in sections that are analogous to a table of contents (e.g., lists of encounters, visit status, problem list), and EHRs include consolidated sections for labs, screening results, and outside reports. However, EHRs are limited by the quality of the data entered. Clinicians excessively reliant on “copy and paste” or pre-written phrases can result in redundant, out of date, or generic information (Bowman, 2013).

Emotional and behavioral changes and symptoms may reflect an infant or young child’s physical discomfort or distress and attention to this possibility allows for the development of a treatment plan to address the underlying cause(s).
Chart Review
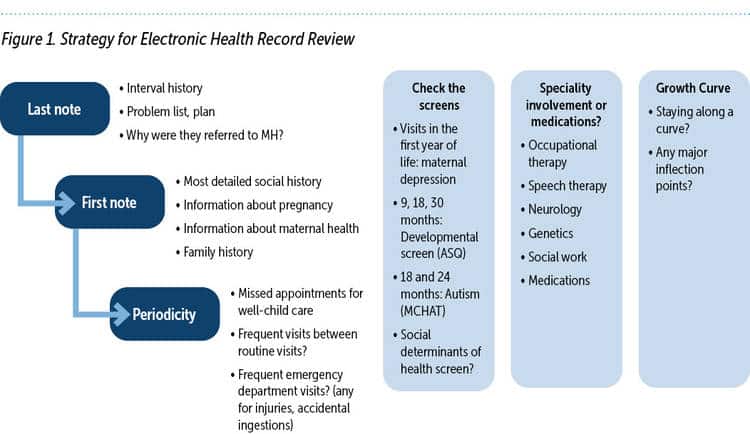
The chart review strategy described here is intended to capitalize on the strengths of most EHRs and highlight some of the highest yield elements of the health record in contributing to Axis III diagnoses. In this way, IECMH professionals, especially those without a physical scope of practice, can quickly, confidently, and efficiently find relevant information. Using this strategy, the chart review begins with the most recent note, then the problem list, and then the first note. This EHR review continues with scanning well-child visit periodicity and screening, checking for visits with selected specialists or settings, the child’s growth curve, and medications. (See Figure 1.)
MOST RECENT NOTE
The most recent note can provide valuable information about the child’s recent health history, document any medications or current treatment (including psychiatric or mental health), and should reference other health concerns. Depending on the timing of the referral and who made the referral, the last note by that provider may explain the reason for the referral for an IECMH evaluation, if one was made.
PROBLEM LIST
The problem list is a cumulative list of clinically significant problems addressed in the pediatric setting. While the list has the potential to be comprehensive, it should not be considered exhaustive as not all providers update the list. The problem list generally includes prenatal health issues like prematurity or exposure to alcohol, chronic conditions like asthma or eczema, acute events like fractures or burns, and contextual factors like being in foster care. The problem list may not be comprehensive, but everything included is valuable.
DC:0–5 delineates examples of the kinds of chronic conditions that may be relevant to the IECMH evaluation because of the direct effects on the child, the indirect effects on the child or family, or the change in a caregiver’s internal working model or representation about the child. Table 2 expands that list by providing some examples of how physical health conditions might influence the IECMH evaluation. A blank problem list may indicate a healthy child with typical development (or lapses in documentation).
First Note
In pediatric charts, often the first note is the discharge note from the baby’s delivery, which offers rich information about physical health and social history. The note, which may be from an outside delivery center and scanned into the pediatric chart, should include information about the pregnancy, the delivery, and the baby’s health status at birth. (See Table 3, p. 76) Pregnancy information includes information relevant to IECMH including physical and mental health of the mother, pregnancy complications, timing of entry into prenatal care, and adherence to recommendations. Late or no prenatal care or limited adherence to obstetric recommendations may indicate other priorities, basic needs deficits during pregnancy, or ambivalence about the pregnancy. Laboratory results offer information about physical health issues (diabetes), prenatal exposure to medications, licit or illicit substances, and sexually transmitted infections. Information about the fetal implications of specific medications can be found on Mother to Baby (mothertobaby.org) or the Center for Disease Control and Prevention’s Treating for Two ( https://www.cdc.gov/pregnancy/meds/treatingfortwo/index.html).
Table 2. Considering the Problem List: Common Pediatric Problems
Family history, whether related to physical health or mental health of the mother or father, may also be included in this record. This information can be particularly helpful if one or more biological parent is not involved at the time of the IECMH evaluation.

Physical health conditions can indirectly influence mental health clinical symptoms through the child or the caregivers’ experiences of the condition.
Typical full-term pregnancies are defined as deliveries between 37 and 42 weeks, with birthweight between 2.5 kg (5 lb 8 oz) and 4.0 kg (8 lbs 13 oz). Babies born preterm or low birthweight may be at higher risk of IECMH concerns, which may be due to central nervous system development, the underlying cause of their preterm birth or low birthweight, and/or contributions of caregiver attributions of their vulnerable child (Vanderbilt & Gleason, 2011). Babies who are transferred to the neonatal intensive care unit or have a prolonged hospital stay may have physical health conditions that may also put them at higher risk of IECMH concerns in the future.
Delivery discharge paperwork may also provide valuable social information about prenatal exposure to interpersonal violence, early involvement of child protective services, or services needed prior to discharge.
Table 3. Interpreting the Newborn Discharge Summary
Pediatric Well-Child Visit Periodicity and Screening
Most EHRs include a list of encounters, often with the visit type and age in the encounter name, for example “4 Month Well-Child.” These lists can offer a quick review of types of health care services a child has received, including adherence to the well-child visit schedule. Table 4 summarizes the expected schedule for well-child visits. Missed well-child visits or late immunizations may indicate that a family has other priorities that supersede attendance at well-child visits, typically related to Axis IV stressors, and are associated with a range of adverse health outcomes (Samuels et al., 2015).
Table 4. Well-Child Visit Checklist
The American Academy of Pediatrics (AAP) also recommends specific timing of psychosocial assessments and screening measures for maternal depression, developmental milestones, and autism spectrum disorder, all of which can provide valuable information about IECMH status. These screens should be available in most EHRs, usually in a consolidated list of test results. It is increasingly common for primary care clinicians to screen for social–emotional well-being in the preschool period using a validated tool (Weitzman & Wegner, 2015). The information from these validated measures may provide a valuable longitudinal picture of the young child and their family from birth to the present. Information about interpreting these measures can be accessed at the AAP Screening Time website (Screeningtime.org).
One of the most important health promotion activities of pediatric primary care is providing immunizations. The abbreviation “IUTD” or “immunizations up to date” is commonly used and provides information about the family’s ability to attend well-child visits in a timely way and the family’s adherence to pediatric recommendations. Not every EHR offers an efficient way for an IECMH clinician to assess whether the immunizations are up to date at a glance, although there may be an alert when a preventive health activity is not documented. These alerts may be helpful for the IECMH clinician in identifying children whose immunizations are delayed or have been declined.
Lab results are generally easy to identify in EHRs. Lead levels and anemia are the two major laboratory results that may provide important information about a child’s IECMH status. Although it is beyond the scope of a non-physical health IECMH clinician to interpret these labs, elevated lead levels may be remarkable as they may be associated with hyperactivity and cognitive delays (AAP Council on Environmental Health, 2016). Both significant anemia, indicated by a low hemoglobin, and elevated lead levels may be related to pica and may also present with mood changes (Lanzkowsky, 2016).
A cornerstone of the pediatric chart is the growth curve, specific for child sex. This curve tracks a child’s growth trajectory compared to other children of the same sex and age from birth to the end of pediatric care. Children’s height, weight, and head circumference (until 24 months old) are measured at each visit and graphed on a chart that includes percentile tracks from 3rd to 97th percentile. Children born preterm are tracked on the basis of their “corrected age” from their expected due date, and a separate growth curve exists for children with trisomy 21 (“Down syndrome”) because of their unique growth patterns (Centers for Disease Control and Prevention, 2000). Although children have some individual variations and may move across a percentile line, generally children will grow “along a curve” and have growth trajectories that fall between the 3rd and 97th percentile. Head circumferences smaller than the 3rd percentile may be related to generalized slow prenatal growth, prenatal exposure to alcohol, a skull disorder in which the bones close early, or slow brain growth that occurs after birth due to genetics or other disorder. Large head circumference is most commonly familial and healthy, but may be associated with autism spectrum disorder or excessive fluid in the brain’s fluid cavities (“hydrocephalus”). Because of the importance of the brain in development and emotional and behavioral regulation, it is helpful to glance at the growth curve to confirm grossly typical head circumference. Growth curves that may be of note for an IECMH clinician include weight curves with a dramatic change up or down across multiple percentile lines or growth above or below the 3rd-97th percentile curves. An IECMH clinician may wonder with a family whether the growth curve inflection points correspond to family stressors or onset of child symptoms. It is worth remembering that young children experiencing food insecurity may present with overweight status rather than underweight in the US (Thomas et al., 2019), likely related to physiologic reactions to inconsistent food access as well as reliance on calorie-dense, inexpensive processed foods.

The most recent note can provide valuable information about the child’s recent health history, document any medications or current treatment (including psychiatric or mental health), and should reference other health concerns.
Notes From Other Encounters or Professionals
A review of a list of clinical notes and visit types also offers a valuable survey of other services a patient may have used. Generally, reading each note is beyond the scope of a pre-visit chart review. However, when an IECMH clinician has time or a particular reason for deeply exploring content of the primary care notes, it is useful to look for a pattern of frequent visits for concerns for which the pediatric intervention is reassurance, which may suggest a higher than usual level of caregiver anxiety or concern for their child’s well-being or for patterns suggestive of factitious disorder imposed on another or medical child abuse. Longitudinal review of notes also may reveal different caregivers who attend visits.
A list of emergency room visits can be reviewed for chief complaints that might reflect caregiving status (e.g., fractures in infants, ingestions of medications or household items, frequent physical injuries). Multiple emergency room or urgent care visits between well-child appointments may indicate limited access to office-based care because of caregiver schedule, transportation, or insurance, or may reflect limited health literacy or caregiver anxiety.
The presence of clinical notes from developmental clinicians like speech and language therapists or occupational therapists may provide insight about a child’s developmental needs, as do notes from neurology or genetics. Certainly, any notes from a mental health professional or care navigator will provide valuable clinical information about the child’s mental health, physical health, and caregiving context.
Medication List
Most EHRs provide an easily accessed list of current as well as past medications. While most medications do not influence clinical symptoms, some medications may contribute to a child’s emotional or behavioral dysregulation, and some children are taking medications specifically intended to support their emotional or behavioral health. It is also possible that a caregiver’s working model of a child may be influenced by the child’s need to take a medication, often by shaping perceptions about the child’s relative vulnerability or resilience. Table 5 summarizes some of the direct effects or adverse effects of common medications as they relate to an IECMH evaluation. IECMH clinicians also always need to ask about both prescribed and non-prescribed interventions, including over-the-counter medications, nutritional supplements, and also cannabinoids that may not have been shared with the pediatric clinician.
Table 5. Commonly Used Medications That May Influence Infant and Early Childhood Mental Health Presentation
Family History
The elements of the family history that are generally included in a pediatric EHR tend to focus on physical health concerns such as asthma and hypertension. Anecdotal evidence suggests that because family history entry in some EHRs can be cumbersome, family histories may be incomplete, especially with regard to the mental health conditions that may influence a child’s functioning through their genetic predisposition or caregiving environment. However, because of the longitudinal nature of the chart, sometimes particularly relevant family history is available, especially about caregivers no longer in the child’s life.
Beyond the EHR
Whether or not a direct review of the EHR is available, caregivers and young children themselves can provide valuable information about Axis III elements through history and observations. In general, the history may be elicited as a chronological narrative beginning with the pregnancy experience, information about the mother and infant’s health in and after the delivery, any chronic medical problems, any illnesses or accidents requiring acute medical attention, concerns about a child’s growth and development, history of surgery or procedures, and any current or long-term medications. During the assessment, observations relevant to Axis III include a child’s apparent size for age and physical proportionality, any dysmorphic features that may suggest a genetic syndrome (e.g., Trisomy 21 or Fragile X) or prenatal exposures (e.g., to alcohol), age-appropriate gross and fine development, movement and interactions that suggest intact vision and hearing, and symmetrical use of arms and legs. Axis III also requires attention to any visible skin conditions that could be causing pain or irritability or evidence of recent or remote non-accidental injury like scars on the back of legs or cigarette burns.
Conclusion
While the positive contributions of the EHR in pediatric and IECMH care continue to be debated, EHRs may offer opportunities for IECMH clinicians to access Axis III-related health information more efficiently than with paper charts. Effective use of the EHR requires a clear appreciation of the relevant health information and a structured approach to eliciting this information. The chart review in no way substitutes for history provided by the family or for the observations of the clinician, but often provides more longitudinal information and sometimes a greater breadth of information than the history and observation alone.
Author Bios
Jennifer M. Moran, PsyD, is a licensed clinical psychologist at Children’s Hospital of The King’s Daughters and an assistant professor of pediatrics at Eastern Virginia Medical School. Her clinical interests include trauma and attachment disorders, depression and anxiety disorders, emotional regulation, identity development and self-efficacy, and school-related concerns. Dr. Moran provides clinical care through evidence-based therapy and assessment services to children, adolescents, and families, as well as program development and implementation. Her research interests include developing interventions and curriculum to promote mental health and well-being in children and adolescents. Her interests also include training mental health, community, and school personnel to implement programs to enhance youth well-being.
Mary Margaret Gleason, MD, is a pediatrician and child and adolescent psychiatrist who serves as vice chair of pediatrics at Eastern Virginia Medical School and vice chief of mental health for Children’s Hospital of The King’s Daughters. She is interested in the clinical care of high-risk young children and their families. In her academic work, Dr. Gleason focuses on early identification of childhood mental health disorders and developing systems of care that bring quality mental health services to young children in mental health settings as well as non-mental health settings. She has developed and validated a screening tool to identify young children at risk for mental health concerns (Early Childhood Screening Assessment) for pediatric practice. She is proud to have served on the Early Brain and Child Development Workgroup of the American Academy of Pediatrics and the Task Force on Integrated Care for the American Academy of Child and Adolescent Psychiatry and to serve on the Board of ZERO TO THREE.
Suggested Citation
Moran, J. M., & Gleason, M. M. (2021). Physical health conditions and considerations in the DC:0–5 diagnostic approach and clinical formulation. ZERO TO THREE Journal, 42(2), 72–79.
References
AAP Council on Environmental Health. (2016). Prevention of childhood lead toxicity. Pediatrics, 138(1), e20161493.
Bell, J. F., Johnson, M. L., Myers, K., & Patrick, D. L. (2010). Primary health care quality in a national sample of children and youth with mental health impairment. Journal of Developmental & Behavioral Pediatrics, 31(9), 694–704.
Bowman, S. (2013). Impact of electronic health record systems on information integrity: Quality and safety implications. Perspectives in Health Information Management, 10(Fall), 1c.
Centers for Disease Control and Prevention. (2000). Clinical growth charts. link
Gleason, M. M., Zamfirescu, A., Egger, H. L., Nelson, C. A., Fox, N. A., & Zeanah, C. H. (2011). Epidemiology of psychiatric disorders in very young children in a Romanian pediatric setting. European Child & Adolescent psychiatry, 20(10), 527–535.
Lanzkowsky, P. (2016). Iron-deficiency anemia. In Lanzkowsky’s manual of pediatric hematology and oncology (pp. 69–83). Academic Press.
Samuels, R. C., Ward, V. L., Melvin, P., Macht-Greenberg, M., Wenren, L. M., Yi, J., Massey, G., & Cox, J. E. (2015). Missed appointments: Factors contributing to high no-show rates in an urban pediatrics primary care clinic. Clinical Pediatrics, 54(10), 976–982.
Thomas, M. M., Miller, D. P., & Morrissey, T. W. (2019). Food insecurity and child health. Pediatrics, 144(4), e20190397.
Vanderbilt, D., & Gleason, M. M. (2011). Mental health concerns of the premature infant through the lifespan. Pediatric Clinics, 58(4), 815–832.
Weitzman, C., & Wegner, L. (2015). Promoting optimal development: Screening for behavioral and emotional problems. Pediatrics, 135(2), 384–395.
ZERO TO THREE. (2016). DC:0–5TM: Diagnostic classification of mental health and developmental disorders of infancy and early childhood.