Rachel Wirtshafter and Diane Lee, Weill Cornell Medicine, New York, New York
Abstract
There is great opportunity in pediatric primary care to lay the foundation for lifelong health and well-being during the critical period from infancy to early childhood. However, many of these opportunities are missed, particularly for the most vulnerable children. The challenges to equitable, universal developmental and behavioral screening in pediatric primary care must be addressed to support the health and well-being of all infants and young children. This article reviews the importance of standardized screening tools for early recognition and intervention of developmental and social–emotional needs as well as the disparities that continue to exist in screening and referral practices. During infancy and early childhood, the brain develops at its fastest rate, with the potential of more than one million neural connections made each second (National Scientific Council on the Developing Child, 2020). Recognizing this crucial age, the American Academy of Pediatrics (AAP) recommended universal early childhood developmental and psychosocial screening (Council on Children With Disabilities et al., 2006). These standardized tools provide low-barrier, evidenced methods for the widespread identification of potential developmental and social–emotional concerns.
As the most universal and accessible setting within early childhood, pediatric primary care is an optimal setting for universal screening. However, a decade and a half after the guidelines were first published by the AAP, significant disparities in screening, diagnosis, and referral rates persist. Despite the availability of validated developmental screening tools across multiple languages, non-English-speaking children, and children of color in general, are far less likely to be screened than White children (Hirai et al., 2018). This disparity in screening is especially concerning because Black children often require a positive screen in order to receive a referral from their pediatrician to early intervention (EI) services while White children are often referred before a positive screen (Wallis et al., 2021). In addition, women from racial and ethnic minority backgrounds, particularly those who are publicly insured, both have the greatest risk for postpartum depression and are the least likely to be screened (Sidebottom et al., 2021). Given that postpartum depression can have long-term adverse developmental, social–emotional, and health consequences, screening is again critical. Together, these findings suggest that sociodemographic factors, rather than developmental or psychosocial risk, play an inequitable role in screening and service referral and that true universal screening could mitigate these disparities.
In the 2 years since the onset of the COVID-19 pandemic, toddlers, especially those from families with low socioeconomic status (SES), have experienced significantly increased incidence of developmental and social–emotional delays (Deoni et al., 2021) as children face increased exposure to traumatic events such as abuse, domestic violence, substance abuse, and increasingly severe maternal depression (Araújo et al., 2021).
The disparities in identification and referrals for developmental and social–emotional delays have important implications for how primary care practices can prioritize equitable care and reduce disparities in screening and referral practices. Evidence-based interventions, such as the HealthySteps program, and quality improvement initiatives hold promise in mitigating disparities. However, many of these efforts have fallen short.
As young children remain out of crucial pre-K programs (Weisenfeld, 2021) pediatricians amass even more responsibility for identifying and intervening in potential developmental and behavioral health concerns. It is now more essential than ever that the challenges to equitable, universal screening in pediatric primary care are addressed to support the health and well-being of all infants and young children. This article reviews the importance of standardized screening tools for early recognition and intervention of developmental and social– emotional needs as well as the disparities that continue to exist in screening and referral practices.
Screening in Pediatric Primary Care
As the medical home, primary care practices are uniquely positioned to identify, refer, and track patients who may be at increased risk for developmental or behavioral health concerns. In 2006, in response to growing concerns that pediatricians were underidentifying developmental delays (DDs) and social–emotional risk factors, the AAP published guidelines recommending the use of evidence-based screening tools (Council on Children With Disabilities et al., 2006). Current guidelines include the administration of standardized postpartum depression screening at 1-, 2-, 4-, and 6-month visits; social–emotional screening annually beginning at birth; and developmental screening at 9-, 18-, and 30-month visits with supplemental screenings at 18- and 24-month visits for autism spectrum disorder (ASD). Developmental surveillance is recommended at all other health supervision visits (Lipkin, Macias, Baer Chen, et al., 2020; Lipkin, Macias, Council on Children With Disabilities, et al., 2020).
Despite evidence of their utility, standardized tools remain underused in pediatric settings, with only 30% of children receiving proper behavior and developmental screening (Keating & Heinemeier, 2022). These screens are used even less frequently with children of color (Morgan et al., 2015), which has contributed to disparities in disorder recognition and treatment across languages and races (Meurer et al., 2022). Even among pediatric offices that have prioritized developmental screening, overcoming inequity has been difficult. For example, despite initiatives which have improved overall screening rates, children who are Black, publicly insured, and living in lower income zip codes maintain significantly lower screening rates than their White, privately insured peers (Meurer et al., 2022).
As a result, preschool children from minority or non-English-speaking backgrounds are significantly less likely to receive a DD diagnosis from their primary care provider (PCP) compared to White children (Gallegos et al., 2021; Rosenberg et al., 2008). Even by the end of middle school, racial and ethnic disparities in DD diagnoses rates persist, leading to decreased access for children of color to special education classrooms and needed classroom adaptations (Morgan et al., 2015). Overall, even though racial and ethnic minorities are at greater risk for developmental and mental health issues (Bowers, 2021), they are the least likely to access needed services. The impact of a missed early diagnosis and lack of needed services can last a lifetime as disparities continue to compound, resulting in lifelong physical and mental health impairments (National Scientific Council on the Developing Child, 2020).
Screening Tools
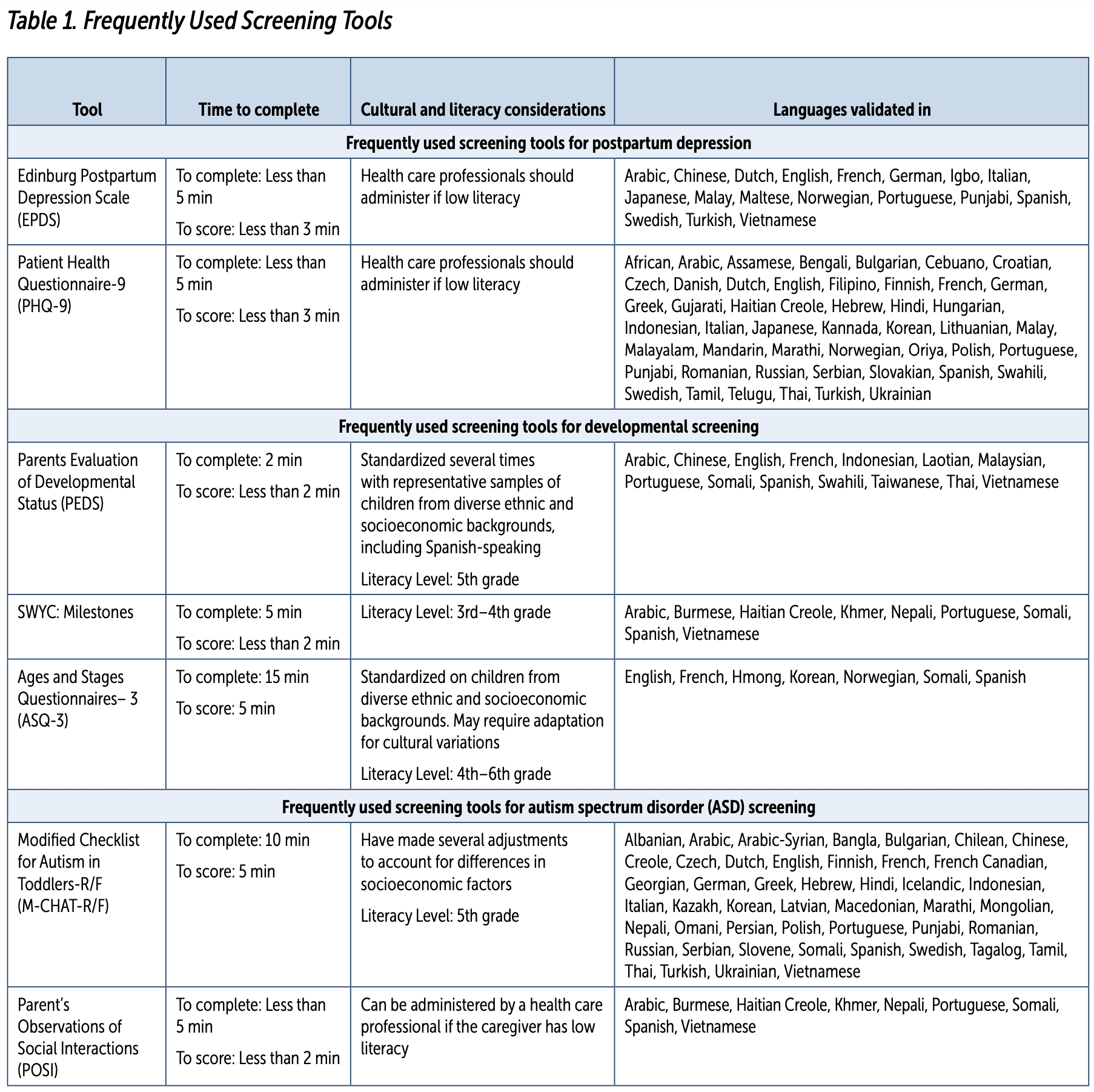
See Table 1 (pp. 48–49) for examples of some frequently used screening tools for postpartum depression, child development, and autism symptoms. Postpartum Depression Screens Postpartum depression screens are currently recommended at 1-, 2-, 4-, and 6-month pediatric visits. The use of standardized postpartum depression screening tools in the primary care setting has led to increased identification and treatment of postpartum depression. However, less than half of pediatricians screen for postpartum depression (Kerker et al., 2016). Given that maternal anxiety and depression symptoms are significant predictors of toddler emotional and social–emotional concerns (O’Connor et al., 2002; Wesselhoeft et al., 2021) it is likely that even before a child reaches their first developmental screen, early risk indicators have already presented to pediatricians.
Sources:
Earls, M. F., Yogman, M. W., Mattson, G., Rafferty, J., & Committee on Psychosocial Aspects of Child and Family Health. (2019). Incorporating recognition and management of perinatal depression into pediatric practice [Policy statement]. Pediatrics, 143(1), e20183259. https://publications.aap.org/pediatrics/article/143/1/e20183259/37241/Incorporating-Recognition-and-Management-of
Glascoe, F. P. (2013). Collaborating with parents: Using Parents’ Evaluation of Developmental Status (PEDS) to detect and address developmental and behavioral problems. PEDStest.com
Lipkin, P. H., Macias, M. M., Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics, Norwood., K. W., Brei, T. J., Davidson, L. F., Davis, B. E., ...McGuinn, L. J. (2020). Promoting optimal development: Identifying infants and young children with developmental disorders through developmental surveillance and screening [Clinical report]. Pediatrics, 145(1). https://publications.aap.org/pediatrics/article/145/1/e20193449/36971/Promoting-Optimal-Development-Identifying-Infants
Rafferty, J., Mattson, G., Earls, M. F. & Yogman, M. W., & Committee on Psychosocial Aspects of Child and Family Health. (2019). Incorporating recognition and management of perinatal depression into pediatric practice [Technical
report]. Pediatrics, 143(1), e20183260. https://publications.aap.org/pediatrics/article/143/1/e20183260/37306/Incorporating-Recognition-and-Management-of
Robins, D. L., Casagrande, K., Barton, M., Chen, C.-M. A., Dumont-Mathieu, T., &
Fein, D. (2014). Validation of the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics, 133(1), 37–45. https://publications.aap.org/pediatrics/article-abstract/133/1/37/68336/Validation-of-the-Modified-Checklist-for-Autism-in
Sheldrick, R. C., Marakovitz, S., Garfinkel, D., Carter, A. S., & Perrin, E. C. (2020). Comparative accuracy of developmental screening questionnaires. JAMA Pediatrics, 174(4), 366–374. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2760904?resultClick
Schonhaut, L., Armijo, I., Schönstedt, M., Alvarez, J., & Cordero, M. (2013). Validity of the Ages and Stages Questionnaires in term and preterm infants. Pediatrics, 131(5), e1468-74. https://publications.aap.org/pediatrics/article-abstract/131/5/e1468/31289/Validity-of-the-Ages-and-Stages-Questionnaires-in?redirectedFrom=fulltext
Weitzman, C., Wegner, L., Section on Developmental and Behavioral Pediatrics, Committee on Psychosocial Aspects of Child and Family Health, Council on Early Childhood, Society for Developmental and Behavioral Pediatrics, American Academy of Pediatrics, ...Wildman, B. (2020). Promoting optimal development: Screening for behavioral and emotional problems. Pediatrics, 135(2), 384–395. https://publications.aap.org/pediatrics/article/135/2/384/33387/Promoting-Optimal-Development-Screening-for
The Edinburgh Postnatal Depression Scale (EPDS), a popular screening tool, is an effective and low-cost screening tool that has been validated in low-income, Black, and Latina women— populations with higher rates of clinically significant depression than the general population (Tandon et al., 2012; see Table 1). Despite the EPDS’s translation into more than 60 different languages, disparities in usage for non-English speaking families remains (Sidebottom et al., 2021).
Developmental Screens
AAP guidelines include the administration of standardized developmental screen for all children at 9-, 18-, and 30-month visits (Lipkin, Macias, Baer Chen, et al., 2020). Developmental screens are used to identify delays that may otherwise be missed by parents or clinicians (Gabrielsen et al., 2015; Wallis & Guthrie, 2020). Without routine screening, 70% of children with developmental or social–emotional concerns will go undetected before kindergarten (Rice et al., 2014). Clinics with routine screening report identifying developmental delays more frequently and at younger ages (Wallis et al., 2021). In addition, developmental screens are largely available in a variety of languages and validated across multiple cultures (see Table 1). They often take less than 15 minutes to complete and can be completed prior to the appointment or in the waiting room. Despite this, only 63% of pediatricians use standardized screening tools (Lipkin, Macias, Baer Chen, et al., 2020), with non-English-speaking patients being less likely to receive both standardized screening and developmental surveillance (Rodrigues et al., 2016).
ASD Screens
Standardized screening tools for ASD are recommended at 18- and 24-month visits (see Table 1). Identification of ASD in the pediatric office can be difficult due to its relatively low prevalence and atypical behavior which often may not present during a visit (Gabrielsen et al., 2015; Wallis & Guthrie, 2020). ASD screening tools have proved to be a valuable piece in early identification of autism, in some cases decreasing the age of diagnosis by 2 years (Robins et al., 2014). However, most parents of children with ASD will raise developmental
or behavioral concerns 2 years before formal diagnosis (Baio et al., 2018). Although a diagnosis of ASD can be made at 2 years old, the average wait time to diagnosis is 3 years, with significantly longer delays in children from lower income and racial and ethnic minority backgrounds (Aylward et al., 2021). This delay in recognition is more profound in Black and Hispanic children, who are evaluated and diagnosed later than White children (Maenner et al., 2020).
Barriers to Screening
Many potential barriers to screening noted by the AAP in 2006 are still observed today. In order to address low screening rates, it is essential to troubleshoot these known roadblocks.
Provider Barriers
Despite decades of research supporting the use of screening tools, rates of use have remained low. Physicians continue to report a preference for clinical acumen over the use of screening tools (Morelli et al., 2014), a consistently unreliable practice that contributes to inequity (Brown & Wissow 2010). In fact, standardized screening has proven to be a better and more reliable tool for accurately identifying children with developmental concerns compared to physicians (Jonsdottir et al., 2020). Still, pediatricians routinely overestimate their rates of developmental surveillance and screening (Lipkin, Macias, Baer Chen, et al., 2020). This overestimation is especially problematic as physicians consistently provide lower quality health care to low-income and minority patients (Smedley et al., 2001).
Most pediatricians cite lack of time, staff, and reimbursement as barriers to standardized screening (King et al., 2010). However, both pediatricians who do and do not administer standardized screenings cite these barriers (Lipkin, Macias, Baer Chen, et al., 2020), suggesting that while barriers will always exist, it is ultimately a matter of priority. Barriers can also include a lack of education. Many PCPs may be unaware of the limits of their clinical interview and surveillance, including that developmental surveillance alone may miss up to 50% of developmental delays (Lipkin, Macias, Baer Chen, et al., 2020) and that positivity rates on standardized depression screenings can be almost 4 times higher than a clinical interview (Olson et al., 2005). In addition, PCPs may not understand the long-term implications of missed postpartum depression, social–emotional risk factors, and developmental delays. For example, educating providers that delayed intervention is both more expensive and less effective, and that the annual burden of childhood mental health disorders is $10.9 billion (Suryavanshi & Yang, 2016), can help reinforce the importance of early social–emotional screening. Finally, the majority of pediatricians report a lack of confidence in their ability to treat developmental and behavioral issues (McMillan et al., 2017). In the context of the competing demands of a brief well-child visit, it is even more difficult for PCPs to prioritize screening when they are uncertain how to adequately address the developmental and behavioral concerns that screenings may identify.
Administrative Barriers
A consistent barrier to screening is a lack of clear clinic workflow and education to the pediatric practice as a whole. For example, although front desk staff are often the first point of contact for patients and provide the screenings directly to patients, they are often not provided with adequate training on the screenings themselves, the importance of screenings, or how to introduce the screenings or answer questions from families. Also, clinic workflows are often unclear, particularly related to who is ultimately responsible for following up on incorrect, missing, or incomplete screens during the clinic visit, resulting in a diffusion of responsibility.
Furthermore, in clinics with diverse patient populations, it may be difficult to have all the required languages for screens on hand. Staff and providers may also be unaware of all the languages in which a screen is available, resulting in providers simply not completing the standardized screenings or using interpreters to complete screens despite the existence of standardized, validated translations. However, having and using screens in all available languages is essential. Even if interpretation services are available, screenings should be administered in the patient’s preferred language because using a translation service can impact the reliability of the screen (Kuhn et al., 2021).
For example, in primary care clinics in California, less than 10% of centers offered developmental and ASD screenings in Spanish (Zuckerman et al., 2013). Not using screeners in the appropriate language increases inequity because it encourages the PCPs’ use of personal judgement disproportionately among Spanish-speaking families. It may also be more difficult to transition to completing screeners in the electronic health record (EHR) because the majority of EHRs do not include many of the most-used screening tools in all the languages in which they are validated.
Patient and Societal Barriers
One of the largest barriers to screening children of color and those from low SES backgrounds is decreased access to primary care, including children’s reduced likelihood of attending early infancy physician appointments. As a result, these families have fewer opportunities for early identification and for parents to discuss developmental concerns (Child and Adolescent Health Measurement Initiative, 2021). Even when children and families access primary care, those from minority and lower SES backgrounds also experience additional barriers to screening. For one, patients of color consistently experience lower quality primary care and lower quality of affiliation with their providers (Stevens & Shi, 2003). Families of color are also far more likely to struggle with low health literacy (Child and Adolescent Health Measurement Initiative, 2021), a barrier which lead to missed early ASD symptoms and to not recognizing developmental milestones (Gallegos et al., 2021).
Reliable screening is necessary to increase the identification of potential developmental delays, and ultimately is a tool for improving the timeliness of diagnoses and referral rates.
The Role of Screening in Reducing Inequity
Despite the many barriers to equitable screening, it is critical that true universal screening be prioritized. Developmental screening has proven to be both a feasible and effective tool to reduce disparities and identify developmental concerns earlier across populations. Patients screened are more likely to be referred for EI services compared to those who receive developmental surveillance alone (Lipkin, Macias, Baer Chen, et al., 2020; Marks et al., 2009). Furthermore, children of color are significantly more likely to be referred only following a positive screen (Wallis et al., 2021), suggesting that true universal screening can decrease disparities in referral rates in racial and ethnic minorities.
Overall, the implementation of screening has increased identification of developmental delays and social–emotional concerns (Lipkin, Macias, Baer Chen, et al., 2020; Marks et al., 2009). The role of screening in reducing inequity is multifaceted. For one, screening tools offer some buffer against provider bias as a standardized way for parents to indicate concerns they may have and to ensure that parents are heard. This is especially important for Black and Hispanic children, as providers are more likely to dismiss parental developmental concerns in Black families compared to White families. Furthermore, even when the concern is noted, it is more likely to be attributed to
a social risk rather than a medical one (Tang et al., 2012). Also, providers do not equally elicit parent concerns, as Spanish-speaking and Black families are less likely to be asked about developmental concerns than are White families, even when the child is considered high risk (Guerrero et al., 2011). Screens may also provide education on developmental expectations for parents. After completing the Ages and Stages Questionnaire, the majority of respondents reported having learned about their child’s strengths and challenges (Morelli et al., 2014). Screenings can also be an important tool for improving health literacy as parents of diverse racial and ethnic groups may differ in their beliefs and expectations for developmental milestones (Pachter & Dworkin, 1997).
For providers, especially those with less experience, screening tools can assist with more accurately identifying developmental concerns compared to surveillance alone (Lipkin, Macias, Baer Chen, et al., 2020). Considering low-income, publicly insured patients are disproportionally seen by medical residents, screening can help reduce this disparity in symptom recognition (Zallman et al., 2010). Screening tools can also remove elements of provider biases which may have led to dismissing developmental concerns, a phenomenon most seen with providers treating Black families (Tang et al., 2012).
Recommendations
The challenges to equitable, universal screening in pediatric primary care must be addressed to support the health and well-being of all infants and young children. Despite recommendations for universal screening, rates of developmental screening remain low, particularly for children from racial and ethnic minority backgrounds. Over time, these disparities compound and lead to higher rates of developmental risk, missed or delayed time to diagnosis, and lower usage of services. Although there is great opportunity in the primary care setting for accessible and equitable care, many of these opportunities are missed for the most vulnerable children. Without sustained efforts, disparities will continue to be perpetuated. Opportunities and quality improvement efforts to promote equitable screening and referral practices in early childhood are presented in the following sections.
Technology
Screenings must be integrated into the EHR so that they can be distributed prior to visits. Electronic screening has allowed for screenings to be complete and scored even before PCPs begin their visits, saving valuable time and allowing PCPs to be more proactive in prioritizing developmental and psychosocial issues as needed in response to positive screens. In addition, electronic screening can facilitate scoring and using algorithms to provide decision support for providers. Standardized algorithms for responding to positive screens can help these needs be addressed within primary care and mitigate the barrier of not administering or addressing screens due to provider discomfort. Registries can be created to track and report clinical data related to screening and positivity rates, as well as provider responses. However, in order to use technology as a health equity tool, practices must create policies and invest in having screenings available in multiple languages.
Provider Training and Education
In the context of a busy pediatric primary care clinic and time constraints, it is often difficult to prioritize developmental and social–emotional screening, particularly when the screenings need to be completed in languages other than English or need to be completed with an interpreter, resulting in the disparities documented in the literature. Education must focus on the limits of developmental surveillance, the importance and implications of missed screens, and how pediatricians can address the developmental and behavioral health needs that the screenings may identify. Furthermore, although the Accreditation Council for Graduate Medical Education now mandates that pediatric residents complete a Developmental and Behavioral Pediatrics rotation, the scope of training through this rotation is not necessarily applicable to the primary care setting. Developmental and social–emotional screening must be part of the primary care practices where pediatric residents complete their training, and national graduate medical training organizations should mandate adherence to AAP policies on screening in these clinics.
Clinic-Wide Training
It is essential that all members of the team are trained in the screening workflow. The workflow must be clearly outlined at each step, including establishing the team members who are responsible for assigning the appropriate screening to each patient, distributing the screenings to patients, monitoring missed and incomplete screenings, and reviewing and responding to positive screens. Clinic-wide training related to the importance of screening can also help prioritize the screening workflow despite a busy clinic setting. Providing brief scripts for the purpose of each screening can aid team members who are the first point of contact for families in distributing the screens.

Even among pediatric offices that have prioritized developmental screening, overcoming inequity has been difficult.
Clinic Data
Presenting data regularly can help PCPs understand that, despite their estimations, screening is still far from universal. In our clinic, we provide the monthly screening rate for the EPDS, Ages and Stages Questionnaire, Survey of Well-being of Young Children, and Modified Checklist for Autism in Toddlers. Furthermore, presenting data from our clinic related to racial and ethnic disparities in screening rates provides evidence that our clinical practices are not free from bias. For example, we have found significant disparities in postpartum depression screening in our clinic by preferred language despite the availability of the EPDS in almost every language. Providing these data to providers reinforces that there are disparities in our clinic and that we must recognize and address these disparities in order to provide equitable care.

Developmental screening has proven to be both a feasible and effective tool to reduce disparities and identify developmental concerns earlier across populations.
Screening Passport
A screening passport can track a young child’s developmental and social–emotional screening history and results, much like a vaccine record. Screening passports can first normalize early on the discussion of social–emotional and behavioral health issues that both families and PCPs may be hesitant to address. Also, it is often difficult for families, particularly for families from racial and ethnic minority backgrounds, to know if their child is being screened at appropriate times as recommended by the AAP. Particularly given that racial and ethnic minorities generally receive poorer quality health care, it is important for both families and PCPs to be aware of recommended and missed screenings. Much like vaccine passports which easily identify care gaps and prompt interventions, screening passports can serve the same function.
Team Based Approach
The needs that a PCP must address during a well-visit can be overwhelming. Team-based approaches such as the HealthySteps program are well suited to meet the often-complex psychosocial needs of racial and ethnic minority families and can provide additional support in responding to positive screening. HealthySteps is an evidence-based, interdisciplinary program that integrates a behavioral health provider into pediatric primary care to promote healthy relationships, foster positive parenting, strengthen early social–emotional development, and ensure access to services (healthysteps.org). By integrating another provider who can specifically provide support around developmental and social– emotional screening and needs for the pediatric primary care team, HealthySteps can help prioritize screening by working alongside PCPs to ensure screenings are completed, by providing education related to the importance and implications of screening, and by providing accessible intervention to families within the primary care setting.
A Culture of Promoting Health Equity
Ultimately, these recommendations will be useful only when pediatric practices shift the culture to one of prioritizing and promoting health equity. Rather than continuing the standard of care, which perpetuates disparities, health care providers must take intentional efforts to recognize and mitigate the aspects of their care that are biased and inequitable. Framing screening and referral processes as health equity issues can help prioritize and infuse discussions of health equity into standard clinic practice.
Limitations of Screening
Reliable screening is necessary to increase the identification of potential developmental delays, and ultimately is a tool for improving the timeliness of diagnoses and referral rates. However, even if equitable screening rates were achieved, only a fraction of children are properly referred for a suspected delay (Rice et al., 2014). Studies suggest that even after identification of developmental delays, Black and Hispanic children are both far less likely to receive EI referrals and access services (Rosenberg et al., 2013). This inequity is likely in part responsible for long-term disparities in diagnostic and behavioral outcomes (Gallegos et al., 2021; Rosenberg et al., 2008).
Ultimately, truly reducing persistent inequity in long-term outcomes and treatment of children with developmental and behavioral health needs will require a shift in how society addresses cycles of poverty, health care access, internal biases, and more. Still, addressing the disparities in early childhood screening and referral practices in pediatric primary care is an important first step in working to address inequity. It is only through focused initiatives aimed at reducing disparities experienced by communities of color that these populations will receive the identification, interventions, and care to create a more equitable nation.
Learn More
Developmental Monitoring and Screening
Centers for Disease Control and Prevention
www.cdc.gov/ncbddd/childdevelopment/screening.html
A Policy Statement on the Impact of Racism on Child and Adolescent Health
American Academy of Pediatrics
https://pediatrics.aappublications.org/content/144/2/e20191765
General Resource for Overview of Screening Tools
American Academy of Pediatrics
www.aap.org/en/patient-care/screening-technical-assistance-and-resource-center/screening-tool-finder
Screening Passports
Office of Early Childhood Development
www.acf.hhs.gov/archive/ecd/child-health-development/watch-me-thrive
HealthySteps for Young Children
www.healthysteps.org
Author Bios
Rachel Wirtshafter, MPH, is a public health professional currently working at Weill Cornell Medicine as a pediatric behavioral health program specialist. She earned her graduate degree at Northeastern University and has worked in a variety of roles including direct service, project management, and pro-social marketing. Professionally, Ms. Wirtshafter is especially interested in suicide prevention among high-risk pediatric populations, improving prevention, identification and treatment of precursors to chronic mental illness and substance abuse, and reducing disparities in access to mental health care access among low-income pediatric populations.
Diane Lee, PsyD, is a licensed clinical psychologist and HealthySteps specialist at New York-Presbyterian Hospital/Weill Cornell Medicine. Dr. Lee completed her graduate training at the University of Denver and completed her postdoctoral fellowship with the Irving Harris Program in Child Development and Infant Mental Health at the University of Colorado School of Medicine. Her clinical and research interests are focused on integrated behavioral health services in pediatric primary care; health and mental health disparities; and work with infants, young children, and families.
Suggested Citation
Wirtshafter, R., & Lee, D. (2022). Toward truly universal screening: Addressing disparities in early childhood screening in pediatric primary care. ZERO TO THREE Journal, 43(1), 46–54.
References
Araújo, L. A. de, Veloso, C. F., Souza, M. de C., Azevedo, J. M. C. de, & Tarro, G. (2021). The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. Jornal de Pediatria, 97(4), 369–377.
Aylward, B. S., Gal-Szabo, D. E., & Taraman, S. (2021). Racial, ethnic, and sociodemographic disparities in diagnosis of children with autism spectrum disorder. Journal of Developmental and Behavioral Pediatrics: JDBP, 42(8), 682–689.
Baio, J., Wiggins, L., Christensen, D. L., Maenner, M. J., Daniels, J., Warren, Z., Kurzius-Spencer, M., et al. (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR. Surveillance Summaries, 67(6), 1–23.
Bowers, V. (2021). Improving access to behavioral health services for racial and ethnic minority youth. University of Washington Center for Health Innovation and Policy Science Policy Brief. https://depts.washington.edu/uwchips/docs/brief-behav-health-youth.pdf
Brown, J. D., & Wissow, L. S. (2010). Screening to identify mental health problems in pediatric primary care: Considerations for practice. The International Journal of Psychiatry in Medicine, 40(1), 1–19. https://doi.org/10.2190/PM.40.1.a. https://journals.sagepub.com/doi/10.2190/PM.40.1.a
Child and Adolescent Health Measurement Initiative. (2021). Fast facts: 2019-2020 National Survey of Children’s Health. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau.
Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, & Medical Home Initiatives for Children With Special Needs Project Advisory Committee. (2006). Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics, 118(1), 405–420.
Deoni, S. C., Beauchemin, J., Volpe, A., & Dâ Sa, V., (2021). Impact of the COVID-19 pandemic on early child cognitive development: Initial findings in a longitudinal observational study of child health. medRxiv. www.medrxiv.org/content/10.1101/2021.08.10.21261846v1.full.pdf
Gabrielsen, T. P., Farley, M., Speer, L., Villalobos, M., Baker, C. N., & Miller, J. (2015). Identifying autism in a brief observation. Pediatrics, 135(2), e330–338.
Gallegos, A., Dudovitz, R., Biely, C., Chung, P. J., Coker, T. R., Barnert, E., Guerrero, A. D., et al. (2021). Racial disparities in developmental delay diagnosis and services received in early childhood. Academic Pediatrics, 21(7), 1230–1238.
Guerrero, A. D., Rodriguez, M. A., & Flores, G. (2011). Disparities in provider elicitation of parents’ developmental concerns for US children. Pediatrics, 128(5), 901–909.
Hirai, A. H., Kogan, M. D., Kandasamy, V., Reuland, C., & Bethell, C. (2018). Prevalence and variation of developmental screening and surveillance in early childhood. JAMA Pediatrics, 172(9), 857–866.
Jonsdottir, S. L., Saemundsen, E., Gudmundsdottir, S., Haraldsdottir, G. S., Palsdottir, A. H., & Rafnsson, V. (2020). Implementing an early detection program for autism in primary healthcare: Screening, education of healthcare professionals, referrals for diagnostic evaluation, and early intervention. Research in Autism Spectrum Disorders, 77, 101616.
Keating, K., & Heinemeier, S. (2022). State of babies yearbook: 2022. ZERO TO THREE.
Kerker, B. D., Storfer-Isser, A., Stein, R. E. K., Garner, A., Szilagyi, M., O’Connor, K. G., Hoagwood, K. E., & Horwitz, S. M. (2016). Identifying maternal depression in pediatric primary care: Changes over a decade. Journal of Developmental and Behavioral Pediatrics, 37(2), 113–120.
King, T. M., Tandon, S. D., Macias, M. M., Healy, J. A., Duncan, P. M., Swigonski, N. L., Skipper, S. M., & Lipkin, P. H. (2010). Implementing developmental screening and referrals: Lessons learned from a national project. Pediatrics, 125(2), 350–360.
Kuhn, J., Levinson, J., Udhnani, M. D., Wallis, K., Hickey, E., Bennett, A., Fenick, A. M., Feinberg, E., & Broder-Fingert, S. (2021). What happens after a positive primary care autism screen among historically underserved families? Predictors of evaluation and autism diagnosis. Journal of Developmental and Behavioral Pediatrics, 42(7), 515–523.
Lipkin, P. H., Macias, M. M., Baer Chen, B., Coury, D., Gottschlich, E. A., Hyman, S. L., Sisk, B., Wolfe, A., & Levy, S. E. (2020). Trends in pediatricians’ developmental screening: 2002–2016. Pediatrics, 145(4), e20190851. https://publications.aap.org/pediatrics/article/145/4/e20190851/76927/Trends-in-Pediatricians-Developmental-Screening
Lipkin, P. H., Macias, M. M., Council on Children With Disabilities, Section on Developmental and Behavioral Pediatrics, Norwood, K. W., Brei, T. J., Davidson, L. F., Davis, B. E., ...McGuinn, L. J. (2020). Promoting optimal development: Identifying infants and young children with developmental disorders through developmental surveillance and screening [Clinical report]. Pediatrics, 145(1), e20193449. https://publications.aap.org/pediatrics/article/145/1/e20193449/36971/Promoting-Optimal-Development-Identifying-Infants
Maenner, M. J., Shaw, K. A., Baio, J., Washington, A., Patrick, M., Dirienzo, M., . . . Dietz, P. M. (2020). Prevalence of autism spectrum disorder among children aged 8 Years—Autism and developmental disabilities monitoring network, 11 Sites, United States, 2016. MMWR Surveillance Summaries, 69(4), 1–12.
Marks, K., Hix-Small, H., Clark, K., & Newman, J. (2009). Lowering developmental screening thresholds and raising quality improvement for preterm children. Pediatrics, 123(6), 1516–1523.
McMillan, J. A., Land, M., Jr., & Leslie, L. K. (2017). Pediatric residency education and the behavioral and mental health crisis: A call to action. Pediatrics, 139(1), e20162141.
Meurer, J., Rohloff, R., Rein, L., Kanter, I., Kotagiri, N., Gundacker, C., & Tarima, S. (2022). Improving child development screening: Implications for professional practice and patient equity. Journal of Primary Care & Community Health, 13, 21501319211062676.
Morelli, D. L., Pati, S., Butler, A., Blum, N. J., Gerdes, M., Pinto-Martin, J., & Guevara, J. P. (2014). Challenges to implementation of developmental screening in urban primary care: A mixed methods study. BMC Pediatrics, 14(1), 16. https://doi.org/10.1186/1471-2431-14-16. https://bmcpediatr.biomedcentral.com/articles/10.1186/1471-2431-14-16
Morgan, P. L., Farkas, G., Hillemeier, M. M., Mattison, R., Maczuga, S., Li, H., & Cook, M. (2015). Minorities are disproportionately underrepresented in special education: Longitudinal evidence across five disability conditions. Educational Researcher (Washington, DC: 1972), 44(5), 278–292.
National Scientific Council on the Developing Child. (2020). Connecting the brain to the rest of the body: Early childhood development and lifelong health are deeply intertwined. (Working Paper No. 15.) https://developingchild.harvard.edu/resources/connecting-the-brain-to-the-rest-of-the-body-early-childhood-development-and-lifelong-health-are-deeply-intertwined
O’Connor, T. G., Heron, J., Golding, J., Beveridge, M., & Glover, V. (2002). Maternal antenatal anxiety and children’s behavioural/emotional problems at 4 years. Report from the Avon Longitudinal Study of Parents and Children. The British Journal of Psychiatry, 180, 502–508.
Olson, A. L., Dietrich, A. J., Prazar, G., Hurley, J., Tuddenham, A., Hedberg, V., & Naspinsky, D. A. (2005). Two approaches to maternal depression screening during well child visits. Journal of Developmental and Behavioral Pediatrics, 26(3), 169–176.
Pachter, L. M., & Dworkin, P. H. (1997). Maternal expectations about normal child development in 4 cultural groups. Archives of Pediatric and Adolescent Medicine, 151(11), 1144–150.
Rice, C. E., Naarden Braun, K. V., Kogan, M. D., Smith, C., Kavanagh, L., Strickland, B., Blumberg, S. J., & Centers for Disease Control and Prevention. (2014). Screening for developmental delays among young children—National Survey of Children’s Health, United States, 2007. MMWR Supplements, 63(2), 27–35.
Robins, D. L., Casagrande, K., Barton, M., Chen, C.-M. A., Dumont-Mathieu, T., & Fein, D. (2014). Validation of the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics, 133(1), 37–45.
Rodrigues, K. K., Hambidge, S. J., Dickinson, M., Richardson, D. B., & Davidson, A. J. (2016). Developmental screening disparities for languages other than English and Spanish. Academic Pediatrics, 16(7), 653–659.
Rosenberg, S. A., Robinson, C. C., Shaw, E. F., & Ellison, M. C. (2013). Part C early intervention for infants and toddlers: Percentage eligible versus served. Pediatrics, 131(1), 38–46.
Rosenberg, S. A., Zhang, D., & Robinson, C. C. (2008). Prevalence of developmental delays and participation in early intervention services for young children. Pediatrics, 121(6), e1503-9.
Sidebottom, A., Vacquier, M., LaRusso, E., Erickson, D., & Hardeman, R. (2021). Perinatal depression screening practices in a large health system: Identifying current state and assessing opportunities to provide more equitable care. Archives of Women’s Mental Health, 24(1), 133–144.
Smedley, B. D., Stith, A. Y., Colburn, L., Evans, C. H., & Institute of Medicine (US). (2001). Increasing racial and ethnic diversity among physicians: An intervention to address health disparities?—The right thing to do, the smart thing to do. NCBI Bookshelf.
Stevens, G. D., & Shi, L. (2003). Racial and ethnic disparities in the primary care experiences of children: A review of the literature. Medical Care Research and Review, 60(1), 3–30. https://doi.org/10.1177/1077558702250229. https://journals.sagepub.com/doi/10.1177/1077558702250229
Suryavanshi, M. S., & Yang, Y. (2016). Clinical and economic burden of mental disorders among children with chronic physical conditions, United States, 2008-2013. Preventing Chronic Disease, 13, E71.
Tandon, S. D., Cluxton-Keller, F., Leis, J., Le, H.-N., & Perry, D. F. (2012). A comparison of three screening tools to identify perinatal depression among low-income African American women. Journal of Affective Disorders, 136(1–2), 155–162.
Tang, B. G., Feldman, H. M., Huffman, L. C., Kagawa, K. J., & Gould, J. B. (2012). Missed opportunities in the referral of high-risk infants to early intervention. Pediatrics, 129(6), 1027–1034.
Wallis, K. E., Davis Rivera, L. B., Guthrie, W., Bennett, A. E., Mandell, D. S., & Miller, J. S. (2021). Provider responses to positive developmental screening: Disparities in referral practices? Journal of Developmental and Behavioral Pediatrics, 42(1), 23–31.
Wallis, K. E., & Guthrie, W. (2020). Identifying autism spectrum disorder in real-world health care settings. Pediatrics, 146(2), e20201467. https://doi.org/10.1542/peds.2020-1467. https://publications.aap.org/pediatrics/article/146/2/e20201467/36931/Identifying-Autism-Spectrum-Disorder-in-Real-World
Weisenfeld, G. G. (2021). Impacts of COVID-19 on preschool enrollment and spending. NIEER Policy Brief.
Wesselhoeft, R., Davidsen, K., Sibbersen, C., Kyhl, H., Talati, A., Andersen, M. S., & Bilenberg, N. (2021). Maternal prenatal stress and postnatal depressive symptoms: Discrepancy between mother and teacher reports of toddler psychological problems. Social Psychiatry and Psychiatric Epidemiology, 56(4), 559–570.
Zallman, L., Ma, J., Xiao, L., & Lasser, K. E. (2010). Quality of US primary care delivered by resident and staff physicians. Journal of General Internal Medicine, 25(11), 1193–1197.
Zuckerman, K. E., Mattox, K., Donelan, K., Batbayar, O., Baghaee, A., & Bethell, C. (2013). Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatrics, 132(3), 445–453.



