Journal
Breaking the Silence: Towards Increased Awareness and Identification of Perinatal Suicide Risk
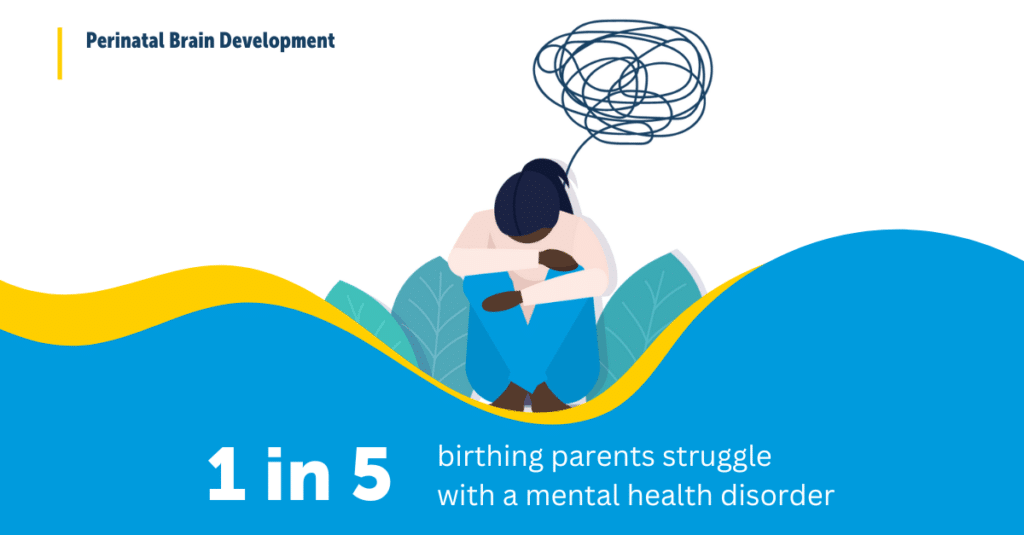
Pregnancy and childbirth mark a transformative period for parents, often celebrated as a time of hope, joy, and new life. However, for many parents, welcoming a baby into the world also comes with unanticipated stress and unique challenges. Although postpartum depression is increasingly recognized as a common experience, another critical perinatal issue remains overlooked: risk for suicide.
Details