Megan E. Carolan and Amber Posey Fishel, Institute for Child Success, Greenville, South Carolina
Abstract
The early childhood workforce encompasses a range of professionals across health care, early childhood education, mental health, child welfare, and early intervention. Despite the differences in daily responsibilities, these professionals experience similar systems-level challenges which impede their ability to professionally flourish and risk undermining the needs of families. In this article, we highlight four key challenges—compensation, burnout, safety, and retention—which have long impacted their sectors and have been further exacerbated by the pandemic. Opportunities for policymakers and program administrators to discuss these challenges are discussed.
Professionals who work with children and their families play many roles, from early childhood education (ECE) providers to social workers to health professionals. While specific responsibilities and training differ, each of these sectors contributes meaningfully to the well-being of children and families, often working with the same families in different contexts. Across these sectors, there are similar challenges facing their workforces, notably: burnout, compensation, safety, and retention. The COVID-19 pandemic moved many of these professionals squarely into the role of “frontline workers”–but often without increasing resources to support them. As policymakers, service providers, funders, and families begin to move forward from this crisis, it is essential to address long-standing issues faced by these workforces and build the resilient, productive, stellar workforce that all children deserve.
Who is a member of the “early childhood workforce?” Traditionally, this term has been used to refer to ECE providers (child care centers, pre-K classrooms, Head Start centers, etc.). In this article, the term is used to comprehensively refer to the broad range of professionals working with young children (up to 8 years old) and families across ECE, health, child welfare, and more. See Box 1 for more details.
Box 1. The Early Childhood Workforce
A comprehensive list of all young professionals working with young children and their families is impossible. This research draws from literature on the following professionals, though the implications for others in related fields are strong:
- early childhood education providers
- teachers (early elementary teachers and special education) and assistant teachers and paraprofessionals
- pediatric medical providers, including doctors and nurses
- mental health professionals, including school counselors and private practice providers (e.g., psychologists, social workers)
- child welfare professionals and home visitors
Why address so many related fields in one conversation? The professionals working in the early childhood sectors have traditionally been discussed in their individual silos: early childhood educators are discussed separately from pediatricians and separate still from social workers, with even further differentiations within these. While distinctions may be necessary for funding streams, regulations, and qualifications, this workforce serves different needs of the same families within a community and faces many similar issues. There are more similarities facing these sectors than it may seem on first glance; by identifying and addressing these challenges at the systems level, there are greater opportunities for progress.
Finally, in a field devoted to children, why focus on the workforce itself? The desired impacts for families and children are simply dreams if systems do not have the qualified, expert workforce to make them real. Investing in the early childhood workforce is tantamount to investing in the people it serves. According to professor James Heckman, Nobel laureate in economics, funding early childhood development amounts to an increase in national economic productivity (Heckman Equation, 2017). To achieve this greater economic impact, there must be a system of adult professionals focused on the health and development of children in all spaces from the doctor’s office to ECE and beyond. These professionals need financial and structural support in the form of professional advancement, substantive wages, access to health care, reasonable caseloads, and more.
Cross-Sector Challenges
This article identifies four key themes prevalent in the literature on individual sectors of the early childhood workforce, with the goal of identifying cross-cutting challenges that require systems-level solutions. This discussion serves as a starting point to identify challenges limiting the impacts of the early childhood workforce; this is not, however, a comprehensive analysis of all professionals.
Compensation
Quality early childhood services require well-trained, committed, and caring professionals, and yet their wages have historically taken a back seat. Early childhood educators frequently leave ECE centers and family home settings for positions in public schools where higher wages and benefits are offered for doing the same or similar work, according to a survey from the National Association for the Education of Young Children (2021). The same can be said for pediatric nurses leaving public school settings to receive better pay and benefits from a position within a hospital system (Vestal, 2021; Willgerodt et al., 2018). When this is the case, professionals may stay within the field but move among employers in search of a better fit for themselves, contributing to turnover or “churn.” Table 1 highlights median salaries for a range of professions focused on young children compared to peers serving adult and older child populations.
Salary is only one component of compensation. Benefits access—sick and vacation time, health insurance, and retirement accounts—vary significantly not only by job type in the field but by employer as well. For example, the vast majority of child life professionals in a recent survey had access to health care benefits (Association of Child Life Professionals, 2020a), while only between 40% and 50% of ECE providers have this benefit (Center for the Study of Child Care Employment, 2021). For doctors and nurses, benefits access differs based on employment settings, with hospital systems the most likely to provide them compared to smaller practices; similarly, child welfare professionals may find a significant difference in benefits provided by working for government agencies directly when compared to nonprofit organizations.
Table 1. Median Salaries for a Selection of Child- and Non-Child Focused Careers
Sources: U.S. Bureau of Labor Statistics, 2020, except where noted; *Association of Child Life Professionals, 2020a; **Incredible Health, 2022; ***National Association of School Psychologists, 2021.
Burnout
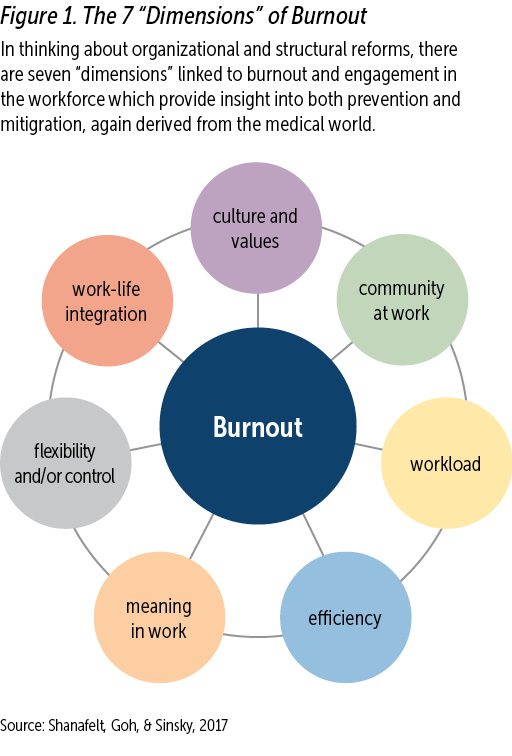
Burnout is defined by the Mayo Clinic (2021) as “a state of physical or emotional exhaustion that also involves a sense of reduced accomplishment and loss of personal identity” (para. 1). It leads to a range of negative physical, mental, and professional impacts (Shanafelt et al., 2017); in the early childhood workforce, burnout could undermine intended benefits for families and children. Among physicians, burnout is associated with depression, relationship difficulties, substance misuse, and even suicide (Shanafelt et al., 2017). Unaddressed burnout has implications for organizations and their staff. Burnout among physicians is linked to intent to leave their current position in the next 2 years, driving very high costs to replace their positions. Turnover of one member of a care team increases the risk of other members of that team leaving, even if a replacement is hired (Shanafelt et al., 2017). Crucially for families, burnout and decreased quality of care are intertwined, though it can be hard to say which causes the other.
Professionals can also be deeply impacted by the experiences of others with whom they work. Secondary traumatic stress (STS) is defined by the National Child Traumatic Stress Network (NCTSN; 2016) as “emotional duress that results when an individual hears about the firsthand trauma experiences of another person” (para. 2). Individuals experiencing STS may feel negativity, detachment, and hopelessness. Much has been written about the experience of social workers and other human service professionals facing STS and similar challenges, but all providers who work with children may experience these feelings as they work with populations facing challenges or struggling emotionally. Struggling with STS is even more likely as families navigate the negative emotional and financial impacts of COVID-19; providers from physicians to teachers may experience their difficulties vicariously while themselves navigating the complexities of the last several years.
STS can impact organizations, not just individuals. NCTSN reported that agencies impacted by STS may become avoidant of these issues, resulting in communication breakdowns that leave staff and clients alike feeling abandoned or ignored (NCTSN, 2016). While the NCTSN guidelines are specific to child welfare organizations, providers who work extensively with clients facing trauma–for example, physicians who work specifically with terminally ill children or ECE providers working in neighborhoods experiencing violence—could also be impacted.

The desired impacts for families and children are simply dreams if systems
do not have the qualified, expert workforce to make them real. Photo: Colors United/shutterstock
Safety
Safety concerns exist in the day-to-day practice of many early childhood-focused professions. Of the 25,000 workplace assaults reported annually, three quarters occur in health care and social service settings, with many assaults never reported (The Joint Commission, 2021). A common scenario for health system violence is when a loved one of a patient attacks a staff member out of fear, stress, or anger (Stephens, 2019). It is easy to imagine such a scenario playing out when a child is critically ill. Child welfare professionals have long advocated for safety protocols. These professionals work with families during unique periods of stress and fear, heightened by suspicion of the home visitor and fear of potential removal of a child from the home. These interactions happen within the client family’s home, an atmosphere outside of the control of the home visitor and without immediate resources such as security to intervene. Safety protocols are often designed regarding physical safety, and not the mental and emotional well-being of workers. Valuable precautions include stress-relieving exercises, employer-provided counseling, or access to mental health services through an insurance plan.
Retention
Retention is essential in any profession that values long-term quality care and is closely linked to the issues of compensation, burnout, and safety previously discussed. The early childhood workforce operates most effectively when it can provide safe and reliable services that address the educational, psychological, and physical health of the most vulnerable population. Operating effectively requires individuals who are highly trained and competent, requiring years of learning, practice, financial investment and passion.
Recruitment and retention are two sides of the same coin. Organizations may struggle with identifying enough qualified applicants for open positions; may face turnover based on employee perception of the difficulty of the work, the quality of management, the hours, the pay, and the general work environment; may find that employees are not performing to their expectations; and may experience waves of retirements based on the age of staff. The pandemic has triggered a significant shift in employment trends. Health care, education, and social services were all impacted by immediate contractions early in the COVID-19 pandemic. While many sectors recovered to pre-pandemic levels by end of 2022, nursing/residential care and education jobs continued to lag (320,000 and 270,000 fewer than in February 2020, respectively; Pickert & Saraiva, 2023). It is a complex scenario, with governments and private industries reducing their investments in these sectors and potential employees turning to other pursuits because of burnout, health concerns, and low pay.
Opportunities
There is no magic wand that can address all of these challenges in one fell swoop; even significant additional funding, which could go a long way to fixing these struggles, would require time and strategic investment. However, many opportunities for leverage exist at the macro policy level as well as within individual programs and employers.
Policy-Level Changes: Increase Compensation
Simply put, professionals working with young children and their families are generally underpaid compared to peers in similar fields. Private ECE providers have average pay on par with dog walkers (Fry, 2020) and even those with specialized degrees working in state-funded programs in schools may be paid less than colleagues who teach older grades in the same buildings (McLean et al., 2017). While pediatricians earn an order of magnitude more than do ECE providers, they are among the lowest compensated of all physician specialties. Similar disparities can also be seen based on pediatric health care and child welfare settings (National Association of Social Workers, New York City Chapter, 2014). While different positions should continue to compensate for differing skill sets and workloads, often professionals are incentivized to jump from one position to another as the best opportunity for a significant salary advance. Reducing this turnover can help stabilize the workforce and improve quality as expertise is developed.
The issue of a pay gap along gender and racial/ethnic lines across all sectors is well documented, even if the causes are complex. Across all backgrounds, women earn 83 cents per dollar compared to White men. Latina women earn 57 cents to every dollar earned by White men, while Black women earn 64 cents to non-White male counterparts (National Women’s Law Center, 2021). The sectors discussed in this article are generally female-dominated and have significant numbers of Latina and Black women, which brings these economic inequalities to light at the macro level.
Increasing compensation across these fields would more fairly compensate employees based on the true value of their labor, particularly given the societal benefits of healthy child development; it could also reduce turnover (and its cost to employers), decrease the high utilization rate of public benefits among these professionals, and improve quality of the services families receive. However, compensation cannot be increased by raising charges for families receiving services. Parents already pay, on average, about 10% of their annual income for child care, significantly higher than the federal definition of affordability (Malik, 2019). Families with health insurance spend $22,000 per year in premium costs (KFF, 2021). Rather, there must be structural changes to the compensation structures in these fields.
Policy-Level Changes: Preparing for Growth
Retaining employees at the current level is a necessary but insufficient step to stabilize employment in these fields. The U.S. economy has a projected job growth rate of 8% between 2020 and 2030 (U.S. Bureau of Labor Statistics, 2021). However, jobs predominantly focused on child well-being exceed that: social workers are projected to experience growth at 12%, and ECE providers at 18%. Pediatricians are in limited supply compared to their growing demand. Enrollment and interest in pediatric subspecialties have slowed to a rate between 20–40% fewer applicants to open positions (Pierce & Stevermer, 2021).
The field of pediatric mental health professionals is of particular concern. In 2021, psychologists reported an increase of 30% in the demand of services for children under 13 years old (Jenco, 2019) yet this field faces several challenges to meet demand, as shown in Box 2.
Many factors explain the growth in need for mental health professionals for children versus adults, such as the COVID-19 pandemic which created a great mental and emotional toll on children who lack the social and emotional development to process the trauma of sudden isolation from their peers, fear amongst their community, and the looming threat of sickness. In particular, the ongoing lack of expertise among providers in handling infant and toddler mental health needs can impact child well-being long-term.
Box 2. Projected Growth in Child Psychiatry
The American Academy of Child and Adolescent Psychiatry recommends 47 child psychiatrists for every 100,000 patients.
- The U.S. averages 9.75 child psychiatrists per 100,000 patients.
- 70% of American counties have no child psychiatrists.
- Few providers have expertise in infant and toddler mental health.
Sources: Jarvis, 2022; Jenco, 2019; Substance Abuse and Mental Health Services Administration, 2020
Employees must be retained while serious investments are made to prepare the workforce of the future, focusing on the “pipeline” from higher education into the field. There is no one solution to the issue of ensuring adequate numbers of high-quality staff across these fields, and the exact education and licensing of each will require its own consideration. Addressing the issues detailed in this article–low compensation compared to peers in related fields; safety concerns that make positions less appealing; and high burnout levels due to emotionally intense work without adequate support–are all important steps to ensure that these professions are attractive to future workers. The conversation must go deeper to consider training for these fields, including the financial costs of higher education and how professionals are recruited into these academic pursuits.
Policy-Level Changes: Data-Driven Decision-Making
Across all sectors discussed in this article, more quality data collection is needed regarding compensation levels, retention and turnover, professional development opportunities, workplace satisfaction, safety concerns, and work-life balance. Some questions posed were nearly impossible to answer, such as which non-salary benefits were available and to whom, or what recent pre-pandemic turnover levels looked like in specific professions. Data on the demographics of these workforces were also relatively difficult to come by, including gender, age, racial/ethnic, and geographic distributions–all of which have implications for equity not only for the workforce itself but also for the families served. When these data points were available, they were often collected as part of academic research studies; these are tremendously beneficial for the field but also risk missing large portions of the professional population depending on the availability and interests of researchers. Alternately, such data may be collected by individual employers (particularly large health care systems) to understand employee needs but are not able to be linked to broader trends in the field to help inform the systems-level changes that are needed. Increased investment in collecting data on these workforces, both from public and private funding sources, is essential to being prepared for the future.
Employer-Level Changes: Creating Conditions to Avoid Burnout
The causes and consequences of burnout are best addressed at the systems level, and not through focusing on advice for individual employees. Specific actions that organizational leadership can take include fostering ongoing communication among staff; creating opportunities for staff to weigh in on work conditions and improvements; focusing on career development; and acknowledging good performance (Shanafelt et al., 2017). Small steps taken to acknowledge, care for, and decrease the stress level of staff can improve experiences at every level from employee to client. In this way, the well-being of individual staff and the workforce as a whole is closely linked to the health of an organization. Burnout is a multifaceted issue; see Figure 1 for a helpful framework provided by Shanafelt, Goh, & Sinksy (2017).

Burnout and decreased quality of care are intertwined, though it can be hard to say which causes the other. Photo: Ground Picture/shutterstock
NCTSN recommends employers find ways to keep staff “tuned in” to their motivations for the work and clearly recognize the positive impact they have on families to help mitigate feelings of burnout (NCTSN, 2016). Organizations should also not overlook changes to their culture which can help create an environment where self-care is the norm. These include allowing and encouraging flexible schedules to the extent possible, encouraging taking an actual lunch break rather than working through it, and setting and honoring boundaries between work and life. It is not enough to simply state these policies in an employee handbook; rather, they must be lived values.
Employer-Level Changes: Professional Development
Professional development (PD) also provides an opportunity for creating meaning and satisfaction within the everyday experiences of service providers, which can help avoid burnout and provide meaningful paths to advancement. Ensuring providers receive opportunities for PD may help improve “compassion satisfaction” which is defined as the positive emotions experienced from helping someone. Broadly, creating opportunities for staff to connect with their motivation for the work and focus on victories (and not just challenges) in the work can help to foster this, which provides a protective factor against burnout (Erdman et al., 2020). Virtual PD should include robust opportunities to connect, receive supportive feedback, and express emotion or else face a higher risk of emotional exhaustion if attendees are only receiving information without being able to fully engage (Roberts et al., 2019).
PD also invests in the professionalization of these fields and can potentially provide opportunities that can reduce burnout and/or isolation among professionals. A catalog of courses is not sufficient to meet professional development needs; high-quality, engaging, research-informed PD must be made available and easily accessible at low/no cost; across geographic locations, or virtually; with cultural and linguistic considerations for both providers and the families they serve. Administrators and program directors must avoid the temptation to schedule classes on self-care or burnout which focus on individual-level strategies only. These can never be sufficient to address the system-wide and cross-sector challenges within these fields.

The early childhood education workforce operates most effectively when it can provide safe and reliable services that address the educational, psychological, and physical health of the most vulnerable population. Photo: Krakenimages.com/shutterstock
Employer-Level Changes: Peer Support
Peer support has been essential for early childhood professionals during the pandemic, particularly in navigating rapid changes to the scope of practice and location, the emotional toll of the work, and safety concerns. From nurses to child welfare providers, professionals identified connecting with their colleagues to share challenges as a valuable resource (NCTSN, 2016). One study among child welfare professionals found the majority of staff shared work-related stressors, positive experiences, and virtual social/community activities with colleagues during the pandemic (He et al., 2020). Among child-life specialists, nearly 3 times more respondents reported seeking support from colleagues than from professional help, suggesting a rich opportunity for formal peer support (Association of Child Life Professionals, 2020b).
Colleagues in the field provide an important support network that can buffer stressors; however, turning to peers for support who are also “pouring from an empty cup” in terms of their own burnout may create a cycle of negativity or even secondary trauma. Formalizing peer learning communities and providing structured opportunities for this sharing, rather than just counting on “water cooler” conversations, can help ensure all participants are supported.
Employer-Level Changes: Embracing Virtual Opportunities
Many of the professions in the early childhood sector require face-to-face, dynamic, and responsive interactions. Historically, the focus has been on providing such interactions in person; but the sudden emergence of the pandemic introduced opportunities to adapt to virtual opportunities. While virtual work would be inappropriate to replace all engagements in these fields, the unprecedented crisis of COVID-19 has created long-term interest in moving some tasks online, including staff meetings, trainings, and a portion of client/patient engagement (Government Accountability Office [GAO], 2021; He et al., 2020).
Telehealth services were heavily utilized during the pandemic to reduce in-person contact for many health care appointments; interest in these virtual appointments has continued for many patients and providers. Early research on trends in telehealth use found that telehealth patients were more likely to be non-Hispanic and White, younger, more likely to live in a low-income community, and more likely to have insurance (Pierce & Stevermer, 2020), leaving a gap in coverage for the many community members existing outside of those classifications. Of particular concern for the future of telemedicine is the continued challenge of Internet accessibility in rural communities (American Academy of Family Physicians Foundation, 2020).
All early childhood fields must develop guidance on the appropriate uses of virtual technology in reaching more families, particularly in health care and child welfare, where state and federal laws may govern privacy expectations (GAO, 2021). Notably, in some fields, a switch to remote work was identified as a major supportive factor during the pandemic which improved employee well-being: in a survey of child welfare providers, the majority expressed that even 1 to 2 days per week of remote work could improve their overall job satisfaction (He et al., 2020; Sisk et al., 2020).
Employer-Level Changes: Safety Considerations
Researchers stress that safety protocols should be central for any child welfare organization, and the use and effectiveness of these practices should be discussed as part of professional development. See Box 3 for a discussion of surveying to develop safety protocols.
To provide support to clinicians facing burnout and secondary trauma, supervisors must be trained in what these symptoms look like and how to respond. Organizations should also develop protocols for how to handle “critical incidents” which may be uniquely stressful for staff (NCTSN, 2016) including the death of a client/patient/student, a violent incident, or a natural disaster. This response can include both group opportunities to process experiences and more individualized “debriefing” with those professionals who are most closely impacted (National Academies of Sciences, Engineering, and Medicine, 2021; NCTSN, 2016). Reflective supervision is an important technique that both supports high-quality work and mitigates or prevents burnout; it has been studied and used in a range of fields impacting children and families.
Box 3. The Survey Says...
All of the fields addressed in this article could benefit from gauging the experiences and feelings of their professionals as they relate to safety. This could be done on a regular (annual) basis through a survey of staff members. The exact questions to be asked will vary by field, but include issues such as the following:
- Do early childhood education providers feel safe in their classrooms? Have their employers adequately developed and trained staff on policies for violence, fire, natural disaster, and other situations?
- Do medical providers feel adequately protected from patient or family violence? Do they have resources to call if a situation is escalated? Does this experience differ by the location in which they practice? Has COVID-19 changed this experience?
- Do child welfare professionals feel comfortable with protocols in place to record their whereabouts for home visits? If a professional feels unsafe in a situation, do they have access to immediate resources to secure the situation? Are options available for mitigating those dangers long-term (e.g., asking to move visits from a home to a neutral location), and do providers feel comfortable questioning those adjustments?

The causes and consequences of burnout are best addressed at the systems level, and not through focusing on advice for individual employees. Photo: Tyler Olson/shutterstock
Conclusion
Children and families do not magically experience improved outcomes just by simple investments in health, education, and welfare; these impacts are achieved only if they are served by a dedicated and talented workforce well-suited to meet their needs. To deliver on the promise of early childhood investment, the workforce requires competitive compensation in line with their peers and with the value of their work; longterm investment to retain talented staff, including professional development and support for the emotionally intense nature of the work; and a commitment to ensuring their physical and mental safety on the job.
While much is similar in the challenges of these fields, the daily experiences of employees can differ significantly across these professions, and even within them depending on their exact roles. The nuances of each sector in terms of training and education requirements, funding sources, compensation structures, and work environments must all be considered. To this end, it is essential that the voices of professionals on the ground steer conversations on reform and long-term sustainability in their respective careers.
Authors
Megan E. Carolan, MPP, is the vice president of policy research at the Institute for Child Success, a nonprofit research organization which advances human-focused and equity-centered policies, partners, and practices to transform systems that impact young children and their families. Ms. Carolan’s work focuses on early childhood policies, systems-based reform for the benefit of families, and a reconceptualization of the role of extended family to improve child outcomes. She holds a master’s of public policy from Rutgers University.
Amber Posey Fishel is a policy research associate with the Institute for Child Success, based out of Greenville, SC. She previously held the position of associate of operations and finance. Ms. Fishel holds a bachelor’s degree in English from the College of Charleston and has split her professional pursuits across a range of sectors, including in the legal tech industry as an administrative manager, and creative interests, acting as collaborative organizer and content creator in a biannual music and arts festival.
Suggested Citation
Carolan, M. E., & Fishel, A. P. (2023). The early childhood workforce across disciplines: Incorporating experiences from health, child welfare, and education to build a sustainable workforce. ZERO TO THREE Journal, 43(3), 5–13.
References
American Academy of Family Physicians Foundation. (2020). Study examines telehealth, rural disparities in pandemic. www.aafp.org/news/practiceprofessional-issues/20200730ruraltelehealth.html
Association of Child Life Professionals. (2020a). 2020 salary survey. www.childlife.org/docs/default-source/resources/2020-salary-survey.pdf
Association of Child Life Professionals. (2020b). Ongoing impacts of COVID-19 on the child life community: Data collection window, October 5-19, 2020. www.childlife.org/docs/default-source/covid-19/ongoing-impact-of-covid-19-on-the-child-life-community---october-2020-(1).pdf
Center for the Study of Child Care Employment. (2021). State policies to improve early childhood educator jobs: Health & well-being supports. https://cscce.berkeley.edu/workforce-index-2020/state-policies-to-improveearly-childhood-educator-jobs/family-and-income-support-policies/health-well-being-supports
Erdman, S., Colker, L. J., & Winter, E. C. (2020). Trauma and young children: Teaching strategies to support and empower children. NAEYC. Fry, E. (2020, March 16). Why dog walkers make more than childcare and eldercare workers. Fortune. https://fortune.com/2020/03/16/dog-walkers-childcare-eldercare-workers
Government Accountability Office. (2021). Child welfare: Pandemic posed challenges but also created opportunities for agencies to enhance future operations (Publication No. GAO-21-483). www.gao.gov/assets/gao-21-483.pdf
He, A. S., Golieb, K., Keniston, M., Grenier, A., & Leake, R. (2020, November). COVID-19 workforce needs assessment (WNA) cross-site report for workforce excellence public child welfare sites. National Child Welfare Workforce Institute. https://ncwwi.org/slug/covid-19-workforce-needs-assessment-wna-cross-site-report-for-workforce-excellence-public-child-welfare-sites
Heckman Equation. (2017). The Heckman Equation brochure. https://heckmanequation.org/resource/the-heckman-equation-brochure
Incredible Health (2022). Average pediatric nurse salary. www.incrediblehealth.com/blog/pediatric-nurse-salary
Jarvis, L. (2022, November 29). The US needs five times as many child psychiatrists. The Washington Post. www.washingtonpost.com/business/the-us-needs-five-times-as-many-child-psychiatrists/2022/11/29/b9c7e4b4-702b-11ed-867c-8ec695e4afcd_story.html
Jenco, M. (2019). Study: 1 in 5 children lives in county without a child psychiatrist. AAP News. https://publications.aap.org/aapnews/news/13762?autologincheck=redirected
KFF. (2021, November 10). Average family premiums rose 4% this year to top $22,000; Employers boost mental health and telemedicine among COVID-19 pandemic, benchmark KFF survey finds. www.kff.org/health-costs/press-release/average-family-premiums-rose-4-this-year-to-top-22000
Malik, R. (2019, June 20). Working families are spending big money on childcare. Center for American Progress. https://www.americanprogress.org/article/working-families-spending-big-money-child-care
Mayo Clinic. (2021). Job burnout: How to spot it and take action. www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/burnout/art-20046642
McLean, C., Dichter, H., & Whitebook, M. (October 2017). Strategies in pursuit of pre-k teacher compensation parity: Lessons from seven states and cities. CSCCE. https://cscce.berkeley.edu/publications/report/strategies-in-pursuit-of-pre-k-teacher-compensation-parity
National Academies of Sciences, Engineering, and Medicine. (2021). The future of nursing 2020-2030: Charting a path to achieve health equity. The National Academies Press. https://doi.org/10.17226/25982
National Association for the Education of Young Children (NAEYC). (2021). Compensation matters most. NAEYC. www.naeyc.org/sites/default/files/globally-shared/downloads/PDFs/resources/blog/compensation_matters_most.pdf
National Association of School Psychologists. (2021). Workforce & salary information. www.nasponline.org/about-school-psychology/workforce-and-salary-information
National Association of Social Workers, New York City Chapter. (2014). Campaign for equitable salaries. www.naswnyc.org/page/Salaries/Campaign-for-Equitable-Salaries.htm
National Child Traumatic Stress Network. (2016). Secondary trauma and child welfare staff: Guidance for supervisors and administrators. http://www.nctsn.org/sites/default/files/resources//secondary_trauma_child_welfare_staff_guidance_for_supervisors.pdf
National Women’s Law Center. (2021). The wage gap: The who, how, why, and what to do. https://nwlc.org/wp-content/uploads/2021/11/2021-who-what-why-wage-gap.pdf
Pickert, R., & Saraiva, A. (2023). US job growth to slow or even reverse after near-record year. Bloomberg. www.bloomberg.com/news/articles/2023-01-05/us-job-growth-to-slow-or-even-reverse-after-near-record-year?leadSource=uverify%20wall
Pierce, R. P., & Stevermer, J. J. (2021). Disparities in use of telehealth at the onset of the COVID19 public health emergency. Journal of Telemedicine & Telecare, 29(1), 3–9. Doi:10.1177/1357633X20963893. https://journals. sagepub.com/doi/10.1177/1357633X20963893
Roberts, A. M., LoCasale-Crouch, J., Hamre, B. K. & Jamil, F. M. (2019). Preschool teachers’ self-efficacy, burnout, and stress in online professional development: A mixed methods approach to understand change. Journal of Early Childhood Teacher Education, 41(3), 262–283. DOI: 10.1080/10901027.2019.1638851. www.tandfonline.com/doi/abs/10.1080/10901027.2019.1638851?journalCode=ujec20
Shanafelt, T., Goh, J., & Sinksy, C. (2017). The business case for investing in physician well-being. Journal of the American Medical Association Internal Medicine, 177(12), 1826–1832. DOI: 10.1001/jamainternmed.2017.4340. https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2653912
Sisk, B., Alexander, J., Bodnar, C., Curfman, A., Garber, K., McSwain, S. D., & Perrin, J. M. (2020). Pediatrician attitudes toward and experiences with telehealth use: Results from a national survey. Academic Pediatrics, 20(5), 628–635. https://doi.org/10.1016/j.acap.2020.05.004
Stephens, W. (2019, May 12). Violence against healthcare workers: A rising epidemic. American Journal of Managed Care. www.ajmc.com/view/violence-against-healthcare-workers-a-rising-epidemic
Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services. (2020). Qualifications of an infant and early childhood mental health consultant.
The Joint Commission. (2021). Physical and verbal violence against health care workers. Sentinel Event Alert, Issue 59. www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea-59-workplace-violence-final2.pdf
U.S. Bureau of Labor Statistics, U.S. Department of Labor (2021, September 8). New release: Employment projections 2020–2030. www.bls.gov/news.release/archives/ecopro_09082021.pdf
U.S. Bureau of Labor Statistics. (2020). Occupational outlook handbook.
Vestal, C. (2021). School nurse deficit deepens as states seek relief. The Pew Charitable Trusts. www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2021/10/26/school-nurse-deficit-deepens-as-states-seek-relief
Willgerodt, M. A., Brock, D. M., & Maughn, E. M. (2018). Public school nursing practice in the United States. The Journal of School Nursing, 34(3), 232–244. DOI: 10.1177/1059840517752456. https://journals.sagepub.com/doi/10.1177/1059840517752456




